Click here to see all images
December, 2016
Case of the Month
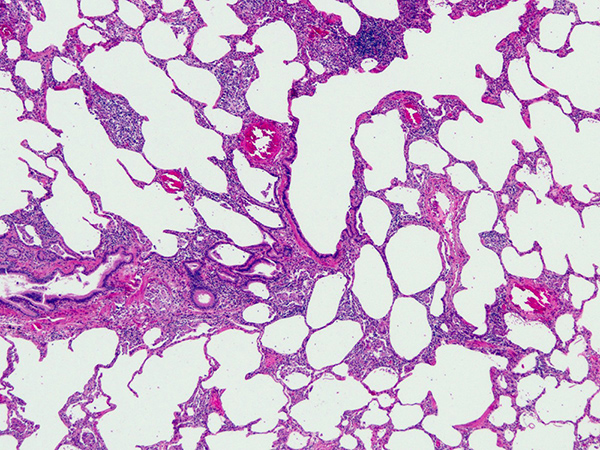
Clinical History:A 53-year-old woman presented with chest tightness and worsening dyspnea on exertion. Spirometry showed restrictive changes. DLCO was 49% on one occasion and 59% on another. Chest CT at another institution was reported as showing “peripheral basilar changes more concerning for NSIP than IPF”. She was a never-smoker. A surgical lung biopsy was performed (Figures 1-6; Fig. 6 shows the same field as Fig. 5 after polarization).
Quiz:
Q1. The predominant cells in this process are:
- Eosinophils
- Granulomas
- Lymphocytes
- Histiocytes
- Macrophages
Q2. What radiologic findings do you expect with these histologic features?
- Honeycomb change and lower zone predominant reticulation
- Tiny nodules in a lymphangitic distribution
- Crazy paving pattern
- Bilateral ground-glass opacities
- Bilateral consolidation and mass-like opacities
Q3. The clinician should seek a history of:
- Exposure to a dusty environment or asbestos
- Working in a coal mine
- Working in a quarry
- Exposure to pet birds
- Exposure to inorganic toxic fumes
Q4. Ideal treatment consists of:
- Smoking cessation
- Azathioprine and/or methotrexate
- Removal of patient from source of exposure, or vice versa
- Pirfenidone
- Corticosteroids
Answers to Quiz
Q1. C
Q2. D
Q3. D
Q4. C
Q2. D
Q3. D
Q4. C
Diagnosis
Hypersensitivity pneumonitis
Discussion
Hypersensitivity pneumonitis (also known as hypersensitivity pneumonia) is a form of interstitial lung disease caused by hypersensitivity to inhaled organic antigens. The diagnosis can be difficult because there is no clearly defined and widely accepted gold standard. In terms of pathology, however, there is agreement regarding what constitutes a classic case, which generally corresponds to a subacute clinical presentation. It is characterized by the following triad: (1) cellular chronic interstitial pneumonia, (2) poorly formed intersitial granulomas and (3) tiny foci of organizing pneumonia.
The "cellular chronic interstitial pneumonia" of hypersensitivity pneumonitis is characterized by the presence of lymphocytes within the interstitium. A few plasma cells and histiocytes may be present. Eosinophils are never prominent. As shown in Figure 1, the infiltrate is slightly more prominent around small bronchioles. In this milieu, a few scattered multinucleated giant cells are often identifiable within the interstitium (Figure 2). Organizing pneumonia, when present, is minimal and inconspicuous. It typically consists of an occasional fibroblast plug within an airspace (Figure 3). Figure 3 also shows a poorly formed granuloma. At high magnification, one can appreciate that the interstitial inflammatory infiltrate is composed mainly of lymphocytes (Figure 4). Multinucleated giant cells often contain non-specific inclusions, which are thought to be endogenous, i.e., products of macrophage metabolism. Cholesterol clefts are especially common, as are microcalcifications. Figure 5 shows a giant cell within the wall of an alveolar duct with a non-specific endogenous inclusion. The same field is shown under polarized light in Figure 6, demonstrating that the inclusion is birefringent. Poorly formed granulomas and/or multinucleated giant cells are typically sparse, and in most cases do not dominate the histologic picture.
Patients are usually never-smokers who present with cough and shortness of breath. Classic radiologic features include bilateral ground-glass opacities, air trapping and mosaic attenuation. Treatment involves removing the patient from the source of exposure or vice-versa. A source of exposure cannot be identified in many cases, but when it can, pet birds are one of the most common offenders. Pathologists must learn to recognize the histologic features of this disease because it is treatable and potentially reversible with appropriate management.
Take home message for traineees: don't expect to find lots of eosinophils in hypersensitivity pneumonitis!
The "cellular chronic interstitial pneumonia" of hypersensitivity pneumonitis is characterized by the presence of lymphocytes within the interstitium. A few plasma cells and histiocytes may be present. Eosinophils are never prominent. As shown in Figure 1, the infiltrate is slightly more prominent around small bronchioles. In this milieu, a few scattered multinucleated giant cells are often identifiable within the interstitium (Figure 2). Organizing pneumonia, when present, is minimal and inconspicuous. It typically consists of an occasional fibroblast plug within an airspace (Figure 3). Figure 3 also shows a poorly formed granuloma. At high magnification, one can appreciate that the interstitial inflammatory infiltrate is composed mainly of lymphocytes (Figure 4). Multinucleated giant cells often contain non-specific inclusions, which are thought to be endogenous, i.e., products of macrophage metabolism. Cholesterol clefts are especially common, as are microcalcifications. Figure 5 shows a giant cell within the wall of an alveolar duct with a non-specific endogenous inclusion. The same field is shown under polarized light in Figure 6, demonstrating that the inclusion is birefringent. Poorly formed granulomas and/or multinucleated giant cells are typically sparse, and in most cases do not dominate the histologic picture.
Patients are usually never-smokers who present with cough and shortness of breath. Classic radiologic features include bilateral ground-glass opacities, air trapping and mosaic attenuation. Treatment involves removing the patient from the source of exposure or vice-versa. A source of exposure cannot be identified in many cases, but when it can, pet birds are one of the most common offenders. Pathologists must learn to recognize the histologic features of this disease because it is treatable and potentially reversible with appropriate management.
Take home message for traineees: don't expect to find lots of eosinophils in hypersensitivity pneumonitis!
References
Barrios RJ. Hypersensitivity pneumonitis: histopathology. Arch Pathol Lab Med 2008;132:199-203.
Coleman A, Colby TV. Histologic diagnosis of extrinsic allergic alveolitis. Am J Surg Pathol 1988;12:514-18.
Hirschmann JV, Pipavath SN, Godwin JD. Hypersensitivity pneumonitis: a historical, clinical, and radiologic review. Radiographics 2009;29:1921-38.
Mukhopadhyay S, Gal AA. Granulomatous lung disease. An approach to the differential diagnosis. Arch Pathol Lab Med 2010; 134:667-90.
Mukhopadhyay S. Pathology of hypersensitivity pneumonitis. Medscape Reference. Updated June 15, 2016. Available at: http://emedicine.medscape.com/article/2078434-overview.
Coleman A, Colby TV. Histologic diagnosis of extrinsic allergic alveolitis. Am J Surg Pathol 1988;12:514-18.
Hirschmann JV, Pipavath SN, Godwin JD. Hypersensitivity pneumonitis: a historical, clinical, and radiologic review. Radiographics 2009;29:1921-38.
Mukhopadhyay S, Gal AA. Granulomatous lung disease. An approach to the differential diagnosis. Arch Pathol Lab Med 2010; 134:667-90.
Mukhopadhyay S. Pathology of hypersensitivity pneumonitis. Medscape Reference. Updated June 15, 2016. Available at: http://emedicine.medscape.com/article/2078434-overview.
Contributors
Sanjay Mukhopadhyay, M.D.
Staff Pathologist
Department of Pathology
Cleveland Clinic, Cleveland, OH, USA
Staff Pathologist
Department of Pathology
Cleveland Clinic, Cleveland, OH, USA