Click here to see all images
December, 2017
Case of the Month
Clinical History: An 81-year-old man presented with generalized weakness and recurrent episodes of melena. Physical examination revealed severe anemia and sensorimotor neuropathy. Upper GI endoscopy showed nodular infiltration of the gastric mucosa in the body and antrum. Peripheral blood smear showed normocytic to microcytic hypochromic RBCs. Serum electrophoresis was negative for an M band. Bone marrow examination showed a mild excess of plasma cells.
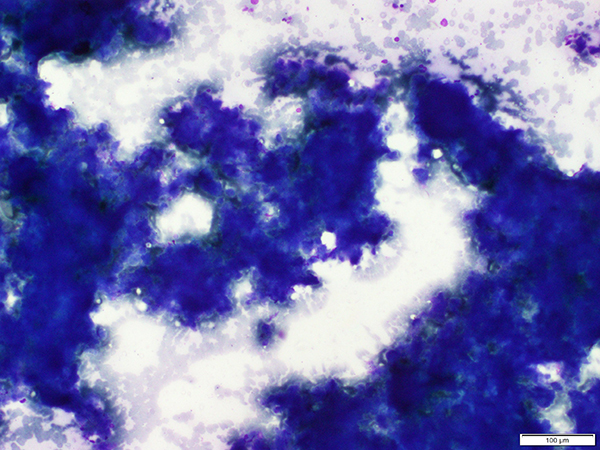
A gastric biopsy showed mucosal infiltration by eosinophilic amorphous material. Later in the course of the disease, the patient developed pleural effusion and was found to have mediastinal lymphadenopathy. EBUS TBNA from the lymph nodes was done (Figures1,2; Figure 1: Giemsa, Figure 2: Congo red). During his hospital stay, the patient developed septic shock with acute kidney injury and succumbed to his illness. Ventilator-associated pneumonia was suspected clinically and a post-mortem lung biopsy was performed (Figures 3-6; Figure 3,4: H&E, Figures 5-6: Congo red).
Quiz:
Q1. Which is not a clinicopathologic form of pulmonary amyloidosisA. Diffuse alveolar-septal
B. Nodular
C. Tracheobronchial
D. Hyalinizing granuloma
E. Localized airway disease
Q2. Which statement is true about the physicochemical composition of amyloid
A. Mostly fibrillar proteins
B. Mostly non-fibrillar proteins and a small portion of P component
C. Soluble fibrillar proteins due to improper folding
D. All branching fibrillary proteins with cross beta configuration
E. Proteins of 8 to 10 micron in diameter
Q3. Which of the following stains needs fluorescence microscopy and is useful for detecting amyloid in tissue sections?
A. Congo red
B.Thioflavin T and S
C. Masson Trichrome
D. Auramine
E. Rhodamine
Q4. The most common clinical manifestation of pulmonary amyloidosis is:
A. Obstructive airway disease
B. Respiratory failure
C. Diffuse alveolar damage
D. Asymptomatic
E. Spontaneous pneumothorax
Answers to Quiz
Q2. A
Q3. B
Q4. D
Diagnosis
Discussion
All amyloid deposits have a similar appearance and staining characteristics under light microscope, consisting of deposition of amorphous acellular material (Figures 3 and 4). Similarly, amyloid proteins share a remarkable physical homology in the form of continuous, nonbranching fibrils of a diameter of approximately 7.5 to 10 nm. Characteristic cross-beta-pleated configuration seen on spectroscopy is responsible for the characteristic Congo red staining and birefringence that is typical of amyloid (Figures 2, 5 and 6).Other stains for detection of amyloid include metachromatic stains (crystal violet and toluidine blue) and immunofluorescent stains (Thioflavin T and Thioflavin S).
However, chemically, amyloid is not a single entity. The 3 most common types of amyloid proteins are AL (Amyloid light chain), AA (Amyloid-associated) and Beta-amyloid protein. Another amyloid protein known as ATTR (Amyloid transthyretin) can accumulate with advancing age or in hereditary amyloidosis.
Amyloid may be localized or systemic. Both AL and ATTR amyloidosis are characterized by multi-system disease. ATTR generally involves the heart and nervous system; often with gastrointestinal symptoms due to autonomic neuropathy. Systemic amyloidosis (AL) involves lungs in approximately 30% to 90% cases but rarely causes significant symptoms. Most cases of localized pulmonary amyloidosis are also due to AL protein. Rarely, AA and ATTR may involve the lungs.
Histologically, there are three types of pulmonary amyloidosis: diffuse alveolar septal, nodular and localized tracheobronchial.
Mediastinal lymph node involvement in systemic amyloidosis is rare. EBUS-TBNA may be an alternative to surgical biopsies for the diagnosis of lymph node involvement by amyloidosis. Cytologically, amyloid appears as amorphous congophilic material (Figure 2) (purple on Giemsa [Figure 1] and light green on Papanicolaou stains).
References
Khoor A, Colby TV. Amyloidosis of the lung. Arch Pathol Lab Med 2017;141:247-54.
Leiro-Fernández V, Botana-Rial M, Represas C, et al. Transbronchial needle aspiration in the diagnosis of mediastinal amyloidosis. Thorax. 2011;66:543.
Contributors
Associate Professor
Department of Pathology
All India Institute of Medical Sciences, New Delhi, India