Click here to see all images
February, 2017
Case of the Month
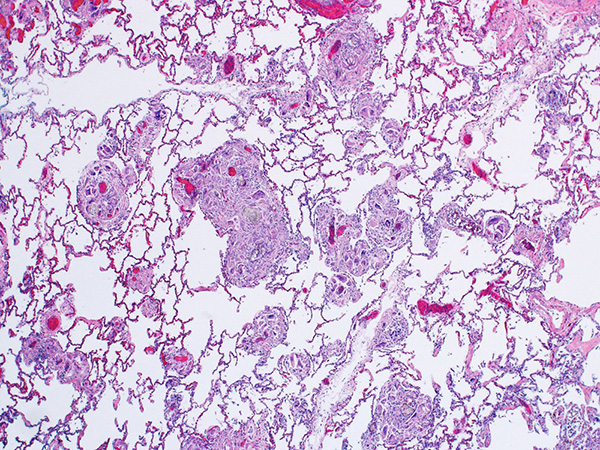
Clinical History:A 42-year-old man presented with increasing dyspnea. Chest CT at an outside institution reportedly showed “interstitial micronodular disease.” An open lung biopsy was performed (Figures 1-6; Fig. 6 under polarized light).
Quiz:
Q1. All of the following pathologic conditions are possible complications of this process EXCEPT
- Pulmonary arterial hypertension
- Interstitial fibrosis
- Hypersensitivity pneumonitis
- Septic emboli
- Abscesses
Q2. The foreign material most commonly seen in lung biopsies in such cases is:
- Microcrystalline cellulose
- Lipid
- Silica
- Beryllium
- Food particles
Q3. The predominant site of injury and inflammation in this process is:
- Perivascular interstitium
- Airspaces
- Small airways
- Subpleural lung
- Large airways
Q4. Which of the following is true regarding the clinical implications of these histologic findings
- The patient should be investigated for sarcoidosis
- The patient is most likely inhaling foreign particles, possibly talcum powder
- The findings are pathognomonic for intravenous heroin abuse
- The findings strongly suggest intravenous injection of oral narcotic pills
- The diagnosis can only be made if there is a clinical history of intravenous drug abuse
Answers to Quiz
Q1. C
Q2. A
Q3. A
Q4. D
Q2. A
Q3. A
Q4. D
Diagnosis
Talc granulomatosis (pulmonary lesions associated with intravenous drug abuse, intravenous talcosis)
Discussion
Pulmonary manifestations of intravenous drug abuse may be caused by direct toxicity of illicit drugs or - as in this case - they may be the result of embolization of insoluble microscopic filler particles to the lung. These particles (also known as excipients) are present within oral tablets, where they have several functions, such as providing bulk to the pill and increasing the bioavailability of the drug. These particles are most commonly encountered in the lung in individuals who inject crushed tablets intended for oral use (mostly narcotics) into their peripheral veins for obtaining a higher and more rapid “high”. Common fillers include microcrystalline cellulose and crospovidone. Historically, talc was used as a filler in oral medications; this is why the terms “talc granulomatosis” or “intravenous talcosis” have been used for this condition. However, currently manufacturers have mostly replaced talc with microcrystalline cellulose.
Embolization of filler particles to the lung elicits a foreign-body granulomatous reaction in the perivascular interstitium. In addition, arterial changes of mild to moderate pulmonary hypertension may be seen, although not all patients develop pulmonary hypertension clinically.
The current case shows patchy nodular expansion of the interstitium by foreign-body giant cells (Figures 1 and 2). The giant cells are located adjacent to small blood vessels in the interstitium, and contain microcrystalline cellulose and crospovidone particles (Figures 3-6). Microcrystalline cellulose particles are large, elongated, rod-like pale-gray crystals on H&E, measuring up to 250 μm in length. They show strong birefringence under polarized light (Figures 4-6). Crospovidone has a deeply basophilic or deep purple coral-like appearance and is not birefringent. It is seen at bottom right in Figures 5 and 6. Talc particles, when present, are smaller (6-23 μm) and sheet-like with a slight yellow hue on H&E and strong birefringence under polarized light.
The most common clinical presentation of talc granulomatosis is worsening shortness of breath. Radiologically there may be evidence of centrilobular micronodules, tree-in-bud opacities, ground-glass opacities and/or pulmonary hypertension. Symptoms and lung injury often progress even after discontinuation of intravenous drug use due to persistence of particulates within the lung. Lung transplantation has been tried in some patients with advanced disease. Given the nature of the illicit activity that leads to these histologic findings, patients often deny intravenous drug abuse and do not always fit the stereotypic profile of a drug addict. Therefore, pathologists should not hesitate to make this diagnosis in the presence of characteristic morphologic features, and should communicate its implications to clinicians.
The differential diagnosis includes aspiration pneumonia caused by aspiration of oral pills. However, the foreign material in such cases is found predominantly in a bronchiolocentric distribution as well as within airspaces, as opposed to talc granulomatosis, where filler particles are found within small blood vessels and in perivascular interstitium. In addition, the presence of intact or degenerated food particles in aspiration pneumonia is helpful in distinguishing the two processes.
Take home message for trainees: Do not hesitate to make a diagnosis of talc granulomatosis in the presence of classic histologic features; a history of intravenous drug abuse will not always be forthcoming.
Embolization of filler particles to the lung elicits a foreign-body granulomatous reaction in the perivascular interstitium. In addition, arterial changes of mild to moderate pulmonary hypertension may be seen, although not all patients develop pulmonary hypertension clinically.
The current case shows patchy nodular expansion of the interstitium by foreign-body giant cells (Figures 1 and 2). The giant cells are located adjacent to small blood vessels in the interstitium, and contain microcrystalline cellulose and crospovidone particles (Figures 3-6). Microcrystalline cellulose particles are large, elongated, rod-like pale-gray crystals on H&E, measuring up to 250 μm in length. They show strong birefringence under polarized light (Figures 4-6). Crospovidone has a deeply basophilic or deep purple coral-like appearance and is not birefringent. It is seen at bottom right in Figures 5 and 6. Talc particles, when present, are smaller (6-23 μm) and sheet-like with a slight yellow hue on H&E and strong birefringence under polarized light.
The most common clinical presentation of talc granulomatosis is worsening shortness of breath. Radiologically there may be evidence of centrilobular micronodules, tree-in-bud opacities, ground-glass opacities and/or pulmonary hypertension. Symptoms and lung injury often progress even after discontinuation of intravenous drug use due to persistence of particulates within the lung. Lung transplantation has been tried in some patients with advanced disease. Given the nature of the illicit activity that leads to these histologic findings, patients often deny intravenous drug abuse and do not always fit the stereotypic profile of a drug addict. Therefore, pathologists should not hesitate to make this diagnosis in the presence of characteristic morphologic features, and should communicate its implications to clinicians.
The differential diagnosis includes aspiration pneumonia caused by aspiration of oral pills. However, the foreign material in such cases is found predominantly in a bronchiolocentric distribution as well as within airspaces, as opposed to talc granulomatosis, where filler particles are found within small blood vessels and in perivascular interstitium. In addition, the presence of intact or degenerated food particles in aspiration pneumonia is helpful in distinguishing the two processes.
Take home message for trainees: Do not hesitate to make a diagnosis of talc granulomatosis in the presence of classic histologic features; a history of intravenous drug abuse will not always be forthcoming.
References
Mukhopadhyay S, Katzenstein AL. Pulmonary disease due to aspiration of food and other particulate matter: a clinicopathologic study of 59 cases diagnosed on biopsy or resection specimens. Am J Surg Pathol 2007;31:752-9.
Shaddy SM, Arnold MA, Shilo K, Frankel WL, Harzman AE, Stanich PP, Singhi AD, Yearsley MM, Arnold CA. Crospovidone and microcrystalline cellulose: a novel description of pharmaceutical fillers in the gastrointestinal tract. Am J Surg Pathol 2016 Dec 22. [Epub ahead of print]
Strickland S, Pena E, Walker AE. Fatal foreign-body granulomatous pulmonary embolization due to microcrystalline cellulose in a patient receiving total parenteral nutrition: all crystals are not what they seem. Forensic Sci Med Pathol 2015;11:255-61.
Tomashefski JF Jr, Hirsch CS. The pulmonary vascular lesions of intravenous drug abuse. Hum Pathol 1980;11:133-45.
Tomashefski JF Jr, Hirsch CS, Jolly PN. Microcrystalline cellulose pulmonary embolism and granulomatosis. A complication of illicit intravenous injections of pentazocine tablets. Arch Pathol Lab Med 1981;105:89-93.
Shaddy SM, Arnold MA, Shilo K, Frankel WL, Harzman AE, Stanich PP, Singhi AD, Yearsley MM, Arnold CA. Crospovidone and microcrystalline cellulose: a novel description of pharmaceutical fillers in the gastrointestinal tract. Am J Surg Pathol 2016 Dec 22. [Epub ahead of print]
Strickland S, Pena E, Walker AE. Fatal foreign-body granulomatous pulmonary embolization due to microcrystalline cellulose in a patient receiving total parenteral nutrition: all crystals are not what they seem. Forensic Sci Med Pathol 2015;11:255-61.
Tomashefski JF Jr, Hirsch CS. The pulmonary vascular lesions of intravenous drug abuse. Hum Pathol 1980;11:133-45.
Tomashefski JF Jr, Hirsch CS, Jolly PN. Microcrystalline cellulose pulmonary embolism and granulomatosis. A complication of illicit intravenous injections of pentazocine tablets. Arch Pathol Lab Med 1981;105:89-93.
Contributors
Mitra Mehrad, M.D.
Assistant Professor
Department of Pathology, Microbiology and Immunology
Vanderbilt University School of Medicine, Nashville, TN, USA
Assistant Professor
Department of Pathology, Microbiology and Immunology
Vanderbilt University School of Medicine, Nashville, TN, USA