Click here to see all images
March, 2017
Case of the Month
Clinical History: A 34-year-old woman with type II diabetes presented with shortness of breath and increasing dyspnea on exertion. After several years of failed medical treatment she underwent lung transplantation. Sections from her explanted lungs are shown below (Figures 1-8).
Q1. Which of the following pathologic findings is indicative of severe pulmonary hypertension
- Chronic interstitial fibrosis
- Plexiform lesions
- Fibrous occlusion of veins
- Congestive changes
- Arterial thrombi
Q2. The histologic findings shown in the preceding images can be caused by all of the following EXCEPT:
- Intravenous drug abuse (talc granulomatosis)
- Alveolar hypoxia
- Right-to-left shunts
- Mixed connective tissue disease
- Pulmonary capillary hemangiomatosis
Q3. Which of the following is true
- In adults, the normal pulmonary artery pressure is 36/27 mm Hg, with a mean of 22 mm Hg
- Histologic findings have an excellent correlation with clinical diagnosis of pulmonary hypertension
- The mean age of patients with pulmonary arterial hypertension in current registries is in the 30s.
- In normal muscular pulmonary arteries, the thickness of the media is 25% of the diameter of the artery.
- Usual interstitial pneumonia (UIP) / Idiopathic pulmonary fibrosis (IPF) is frequently associated with pulmonary hypertension
Q4. In a lung with thick pulmonary arteries, which of the following is a clue to the presence of venous/post capillary obstruction
- Hemosiderin deposition and hemorrhagic infarcts
- Intimal fibrosis of pulmonary arteries
- Muscularization of arterioles
- Plexiform lesions and dilatation lesions (angiomatoid lesions)
- Medial hypertrophy of pulmonary arteries
Answers to Quiz
Q1. B
Q2. C
Q3. E
Q4. A
Q2. C
Q3. E
Q4. A
Diagnosis
Primary pulmonary hypertension (idiopathic pulmonary arterial hypertension)
Discussion
Pulmonary arterial hypertension is diagnosed clinically on the basis of right heart catheterization showing a pulmonary arterial pressure greater than 25 mm Hg at rest or greater than 30 mm Hg during exercise. Thus, the diagnosis of pulmonary arterial hypertension is fundamentally clinical, not pathologic. Pathology plays a role in determining the etiology in some cases.
There are several grading schemes based on clinical, etiologic, and pathologic features. The most straightforward scheme separates cases based on arterial or venous origin. Pulmonary arterial hypertension can be primary or idiopathic, thrombotic/thromboembolic, embolic, or due to left-to-right shunts, collagen vascular diseases, HIV infection, cirrhosis, portal hypertension, chronic fibrosing diseases such as usual interstitial pneumonia (UIP) / idiopathic pulmonary fibrosis (IPF), alveolar hypoxia, and certain drugs. Causes of pulmonary venous hypertension include pulmonary veno-occlusive disease (PVOD), extrapulmonary venous obstruction, and pulmonary capillary hemangiomatosis.
Pulmonary hypertension is graded as mild, moderate or severe. Mild and moderate cases show muscular arteries with medial hypertrophy, variable intimal fibrosis, and muscularization of the arterioles. For a diagnosis of severe pulmonary hypertension, in addition to the above findings one must find either severe intimal fibrosis, plexiform lesions, dilatation (angiomatoid) lesions, or necrotizing arteritis. Plexiform and dilatation lesions are related, and are often found in the same case. Plexiform lesions are glomeruloid proliferations of small, thick-walled vascular channels that appear as outpouchings from muscular arteries, typically just distal to branch points. Dilatation lesions are similar to plexiform lesions but consist of dilated, thin-walled vascular spaces. While not seen in all cases of pulmonary hypertension, plexiform and dilatation lesions constitute definitive histologic evidence of severe irreversible pulmonary hypertension and are considered pathognomonic.
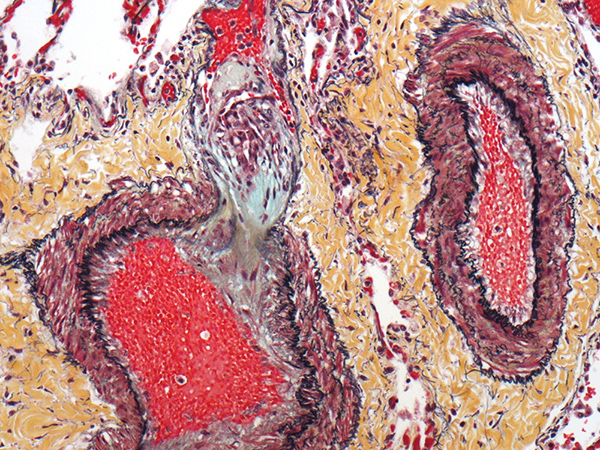
In the current case, Figures 1-8 illustrate medial hypertrophy of muscular arteries with intimal fibrosis, luminal narrowing, muscularization of arterioles, and multiple plexiform and dilatation lesions. These findings, highlighted by Movat pentachrome stains (Figures 1,6, and 7), are diagnostic of severe pulmonary hypertension.
Of note, abnormally thick pulmonary arteries are commonly encountered in lung biopsies from cases of interstitial lung disease, most commonly UIP. In this context, the vascular findings are considered secondary to the chronic fibrotic process, and do not correlate clinically with increased pulmonary arterial pressures.
Take home message for trainees: Pulmonary hypertension is diagnosed clinically based on measurement of pulmonary artery pressures. Do not attempt to diagnose this entity histologically based solely on the finding of thick pulmonary arteries.
There are several grading schemes based on clinical, etiologic, and pathologic features. The most straightforward scheme separates cases based on arterial or venous origin. Pulmonary arterial hypertension can be primary or idiopathic, thrombotic/thromboembolic, embolic, or due to left-to-right shunts, collagen vascular diseases, HIV infection, cirrhosis, portal hypertension, chronic fibrosing diseases such as usual interstitial pneumonia (UIP) / idiopathic pulmonary fibrosis (IPF), alveolar hypoxia, and certain drugs. Causes of pulmonary venous hypertension include pulmonary veno-occlusive disease (PVOD), extrapulmonary venous obstruction, and pulmonary capillary hemangiomatosis.
Pulmonary hypertension is graded as mild, moderate or severe. Mild and moderate cases show muscular arteries with medial hypertrophy, variable intimal fibrosis, and muscularization of the arterioles. For a diagnosis of severe pulmonary hypertension, in addition to the above findings one must find either severe intimal fibrosis, plexiform lesions, dilatation (angiomatoid) lesions, or necrotizing arteritis. Plexiform and dilatation lesions are related, and are often found in the same case. Plexiform lesions are glomeruloid proliferations of small, thick-walled vascular channels that appear as outpouchings from muscular arteries, typically just distal to branch points. Dilatation lesions are similar to plexiform lesions but consist of dilated, thin-walled vascular spaces. While not seen in all cases of pulmonary hypertension, plexiform and dilatation lesions constitute definitive histologic evidence of severe irreversible pulmonary hypertension and are considered pathognomonic.
In the current case, Figures 1-8 illustrate medial hypertrophy of muscular arteries with intimal fibrosis, luminal narrowing, muscularization of arterioles, and multiple plexiform and dilatation lesions. These findings, highlighted by Movat pentachrome stains (Figures 1,6, and 7), are diagnostic of severe pulmonary hypertension.
Of note, abnormally thick pulmonary arteries are commonly encountered in lung biopsies from cases of interstitial lung disease, most commonly UIP. In this context, the vascular findings are considered secondary to the chronic fibrotic process, and do not correlate clinically with increased pulmonary arterial pressures.
Take home message for trainees: Pulmonary hypertension is diagnosed clinically based on measurement of pulmonary artery pressures. Do not attempt to diagnose this entity histologically based solely on the finding of thick pulmonary arteries.
References
Burke AP, Farb A, Virmani R. The pathology of primary pulmonary hypertension. Mod Pathol 1991;4:269-82.
Katzenstein AL. (2016). Diagnostic Atlas of Non-Neoplastic Lung Disease. New York, NY: Springer.
Pietra GG, Edwards WD, Kay JM, et al. Histopathology of primary pulmonary hypertension: a qualitative and quantitative study of pulmonary blood vessels from 68 patients in the National Heart, Lung and Blood Institute, Primary Pulmonary Hypertension Registry. Circulation 1989;80:1198-206.
Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 2013;62:D34-41.
Wagenvoort CA, Wagenvoort N. Primary pulmonary hypertension. A pathologic study of the lung vessels in 156 clinically diagnosed cases. Circulation 1970;42:1163-84.
Katzenstein AL. (2016). Diagnostic Atlas of Non-Neoplastic Lung Disease. New York, NY: Springer.
Pietra GG, Edwards WD, Kay JM, et al. Histopathology of primary pulmonary hypertension: a qualitative and quantitative study of pulmonary blood vessels from 68 patients in the National Heart, Lung and Blood Institute, Primary Pulmonary Hypertension Registry. Circulation 1989;80:1198-206.
Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 2013;62:D34-41.
Wagenvoort CA, Wagenvoort N. Primary pulmonary hypertension. A pathologic study of the lung vessels in 156 clinically diagnosed cases. Circulation 1970;42:1163-84.
Contributors
Yasmeen M. Butt, M.D.
Thoracic Pathology Fellow
Department of Pathology
University of Texas Southwestern, Dallas, TX, USA
Thoracic Pathology Fellow
Department of Pathology
University of Texas Southwestern, Dallas, TX, USA