Click here to see all images
November, 2017
Case of the Month
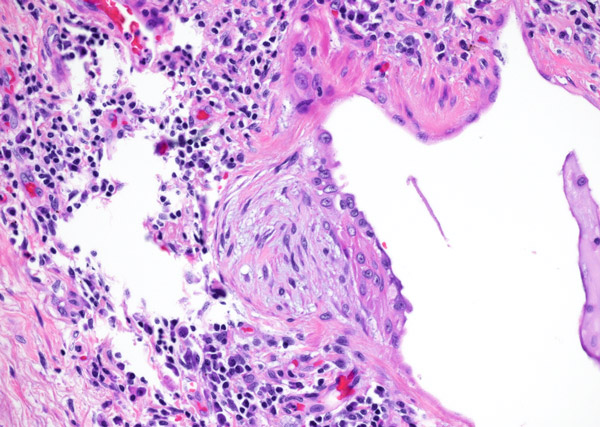
Clinical History: A 75-year-old man presented with increasing shortness of breath and cough. He had been complaining of worsening symptoms for the past year and a half and had been treated with multiple rounds of antibiotics for pneumonia which failed to improve his symptoms. Sections are shown from the right lower lobe (Figures 1-6).
Quiz:
Q1. What is the typical distribution of this disease process?
- Upper lobe predominant with periphery more severely affected.
- Bronchiolocentric (airway) process with upper lobe predominance
- Bronchiolocentric (airway) process with lower lobe predominant
- Lower lobe predominant with periphery more severely affected
- Lymphantic distribution pattern
Q2. Of the following specimen types, which has the lowest yield for this disease?
- Explanted lung
- Transbronchial biopsy
- Cryobiopsy
- Open lung biopsy
- Video-assisted thoracoscopic wedge biopsy
Q3. Which of the following pathologic findings is the best fit for this disease process?
- Loose interstitial granulomas
- Fibroblastic foci at interface between normal and abnormal
- Homogeneous fibrous thickening of septa
- Foci of intra-alveolar giant cells
- Fibrous remodeling of pleura with lymphoid aggregates
Q4. Which of the following features should suggest an alternative diagnosis?
- Honeycombing, predominantly at lung bases
- Mild chronic inflammation
- Fibroblastic foci at interface between normal and abnormal
- Lymphangitic distribution of tightly formed granulomas
- Temporal heterogeneity of fibrosis with foci of normal appearing lung
Answers to Quiz
Q1. D
Q2. B
Q3. B
Q4. D
Q2. B
Q3. B
Q4. D
Diagnosis
Usual interstitial pneumonia (UIP)
Discussion
Usual interstitial pneumonia (UIP) is a fibrosing interstitial pneumonia and is one of the more common interstitial lung disease diagnoses made by the surgical pathologist. It is an important diagnosis not to miss and also not to overcall as it has important clinical consequences (treatment with anti-fibrotics and possible lung transplantation after disease progression). UIP is the pathologic correlate to the clinical term idiopathic pulmonary fibrosis (IPF) and as its clinical moniker implies the cause of UIP/IPF is unknown. It is hypothesized that there is some form of ongoing damage occurring within the lungs to incite a fibrotic response. The fibrosis is more prominent peripherally and in the lower lobes. Histologic features required for diagnosis include temporal and spatial heterogeneity, fibroblastic foci, and honeycombing. Fibroblastic foci are located within the interstitium and most commonly at the border of the advancing fibrosis. They are composed of a proliferation of fibroblasts and their nuclei are usually arranged parallel to the interstitium. They form small outpouchings within the interstitium and can be appreciated on low power by their myxoid appearance (Figure 1). They should be distinguished from fibroblastic plugs which are seen in organizing pneumonia. Fibroblastic plugs look similar but are located within airspaces and not in the interstitium. While fibroblastic foci should be present in order to diagnose UIP (with rare exceptions), it is important to note that they are not specific for UIP and can be seen in other interstitial lung diseases. Honeycombing is another key feature for the diagnosis of UIP. It consists of architecturally distorted airways surrounded by fibrosis and often with inspissated secretions (Figures 2 and 3). In UIP, honeycombing is typically most prominent in the lower lobes and at the bases and less so in the upper lobes. UIP shows a distinctive appearance on lower power of normal-appearing lung juxtaposed with severely fibrotic lung (Figure 4). The fibrotic areas are often most extensive in subpleural parenchyma and along interlobular septa, leaving a donut of normal-appearing lung in the center (“spatial heterogeneity”) (Figures 5 and 6). Temporal heterogeneity refers to differing ages of fibrosis as well as the uninvolved lung as compared to heavily involved lung. A mild chronic inflammatory component is often seen in UIP but if the inflammation is severe and widespread other diagnoses should be considered.
UIP is typically diagnosed with confidence on the following specimen types: explant lung, wedge biopsy, and occasionally on transbronchial cryobiopsy depending on sampling. Transbronchial biopsies do not usually reach far enough out into peripheral lung parenchyma to adequately sample honeycombing. Additionally, these small samples do not typically include the entire constellation of findings required to diagnose UIP with confidence. In cases where UIP can be confidently diagnosed on imaging studies, lung biopsy is not indicated. It is the cases where radiology is unsure about a UIP diagnosis where pathology becomes key to the diagnosis. Additionally, radiology cannot discern microscopic honeycombing, a key feature in UIP as mentioned above.
Take home message for trainees: The diagnosis of UIP requires temporal and spatial heterogeneity, fibroblastic foci, and honeycombing. This diagnosis is very difficult to make on transbronchial biopsies.
UIP is typically diagnosed with confidence on the following specimen types: explant lung, wedge biopsy, and occasionally on transbronchial cryobiopsy depending on sampling. Transbronchial biopsies do not usually reach far enough out into peripheral lung parenchyma to adequately sample honeycombing. Additionally, these small samples do not typically include the entire constellation of findings required to diagnose UIP with confidence. In cases where UIP can be confidently diagnosed on imaging studies, lung biopsy is not indicated. It is the cases where radiology is unsure about a UIP diagnosis where pathology becomes key to the diagnosis. Additionally, radiology cannot discern microscopic honeycombing, a key feature in UIP as mentioned above.
Take home message for trainees: The diagnosis of UIP requires temporal and spatial heterogeneity, fibroblastic foci, and honeycombing. This diagnosis is very difficult to make on transbronchial biopsies.
References
Katzenstein AL, Mukhopadhyay S, Myers JL. Diagnosis of usual interstitial pneumonia and distinction from other fibrosing interstitial lung diseases. Hum Pathol. 2008 Sep;39(9):1275-94.
American Thoracic Society; European Respiratory Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002 Jan 15;165(2):277-304.
Katzenstein AL, Zisman DA, Litzky LA, Nguyen BT, Kotloff RM. Usual interstitial pneumonia: histologic study of biopsy and explant specimens. Am J Surg Pathol. 2002 Dec;26(12):1567-77.
American Thoracic Society; European Respiratory Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002 Jan 15;165(2):277-304.
Katzenstein AL, Zisman DA, Litzky LA, Nguyen BT, Kotloff RM. Usual interstitial pneumonia: histologic study of biopsy and explant specimens. Am J Surg Pathol. 2002 Dec;26(12):1567-77.
Contributors
Yasmeen M. Butt, M.D.
Assistant Professor
Department of Pathology
University of Texas Southwestern, Dallas, TX, USA
Assistant Professor
Department of Pathology
University of Texas Southwestern, Dallas, TX, USA