Click here to see all images
October, 2017
Case of the Month
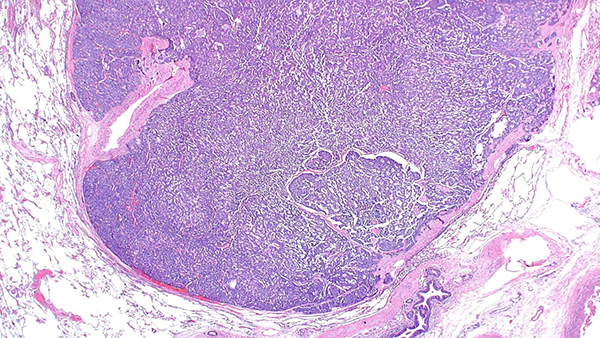
Clinical History: A 61-year-old woman presented with increasing cough and shortness of breath over a 3-month period. She was a never-smoker. Chest CT showed bilateral air-trapping and multiple subcentimeter nodules, the largest measuring 9 mm. She underwent diagnostic wedge resections from the right upper, middle and lower lobes (Figures 1-5, Figures 4 and 6: synaptophysin)
Quiz:
Q1. Which of the following radiologic patterns is not associated with this disease?"
- Mosaic attenuation on expiratory images
- Multiple lung nodules
- Bronchial wall thickening
- Bronchiectasis
- Spiculated nodule
Q2. True or false? This entity can be diagnosed on the basis of pathologic findings without knowledge of the clinical/radiologic setting.
- True
- False
Q3. The predominant site of injury in this process is:"
- Perivascular interstitium
- Airspaces
- Small airways
- Subpleural lung
- Large airways
Q4. Which of the following is true regarding this entity?"
- Most patients have associated MEN 1.
- Ki-67 proliferation index is key in establishing the diagnosis
- Patients often develop high-grade neuroendocrine carcinomas
- Mild lymphocytic inflammation and small airway fibrosis are often seen
- Steroids reverse the course of disease in all patients
Answers to Quiz
Q2. B
Q3. C
Q4. D
Diagnosis
Discussion
Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH) is a rare entity, involving mostly women in the 5th or 6th decade of life. Patients are frequently symptomatic, presenting with cough, shortness of breath, and wheezing. Occasionally, cases are identified incidentally during chest CT imaging for other conditions. The common radiologic findings on high-resolution CT of the chest include nodular bronchial wall thickening, mosaic attenuation caused by mucus plugging, air-trapping on expiration, multiple nodules and bronchiectasis.
Histologic features include proliferation of pulmonary neuroendocrine cells (Kulchitsky-like cells) that may remain confined to the mucosa of small airways, spill into the lumen or extend across the basal lamina to form carcinoid tumorlets (Figure 2) or even carcinoid tumors (Figure 1). Carcinoid tumors and tumorlets are differentiated by a size cutoff of 5 mm. Carcinoid tumorlets embedded within fibrosis can destroy bronchioles, causing obliterative bronchiolitis. Figure 3 shows a small airway partially damaged by granulation tissue and neuroendocrine cells spilling into the lumen. Over time, the granulation tissue within the small airway may be replaced by scarring (Figure 5). These scarred airways can be identified by their location adjacent to a pulmonary artery (Figure 5). The neuroendocrine cells are cytologically bland and have a “salt-and-pepper” chromatin pattern. Immunostains for synaptophysin (Figures 4 and 6) and chromogranin are helpful in confirming the neuroendocrine nature of these lesions.
The differential diagnosis for DIPNECH includes carcinoid tumorlets and neuroendocrine cell hyperplasia. Carcinoid tumorlets (and/or neuroendocrine cell hyperplasia) are common incidental findings in biopsies/resections taken for other lung diseases. In such settings, most authors believe that they are a reactive/secondary phenomenon, and should not be diagnosed as DIPNECH. The diagnosis of DIPNECH requires that the background lung be devoid of pathologic conditions that could explain secondary/reactive neuroendocrine proliferation. Morphologically, the changes in incidental neuroendocrine hyperplasia are similar to DIPNECH, however, fibrous destruction of the airways is not common and overall the features are not as widespread as DIPNECH. More importantly, clinical symptoms and radiographic findings should be appropriate. Thus, DIPNECH is a diagnosis that requires clinicopathologic and radiologic correlation.
Patients with DIPNECH often remain stable, but some suffer from progressive disease leading to respiratory failure. To date, there is no effective treatment. Corticosteroids and octreotide are among the commonly used treatments in these patients, but is unclear whether they improve outcomes. Lung transplantation in selected patients remains the only therapeutic option.
Take home message for trainees: The diagnosis of DIPNECH requires pathologic evidence of neuroendocrine hyperplasia, the absence of background chronic lung disease, and correlation with clinical and radiologic findings.
References
Nassar AA, Jaroszewski DE, Helmers RA, et al. Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia: a systematic overview. Am J Respir Crit Care Med 2011;184:8-16.
Wirtschafter E, Walts AE, Liu ST, Marchevsky AM. Diffuse Idiopathic Pulmonary Neuroendocrine Cell Hyperplasia of the Lung (DIPNECH): Current Best Evidence. Lung 2015;193:659-67.
Contributors
Assistant Professor
Department of Pathology, Microbiology and Immunology
Vanderbilt University School of Medicine, Nashville, TN, USA