Click here to see all images
December, 2018
Case of the Month
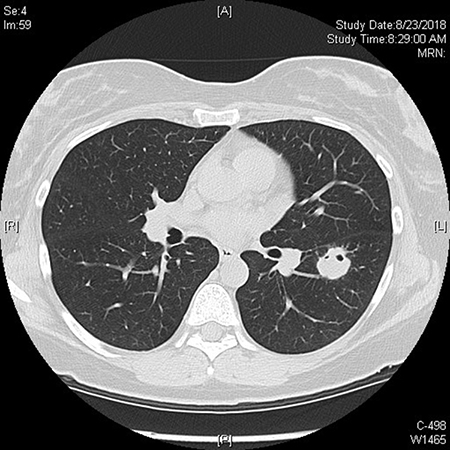
Clinical History: A 2.3 cm left lower lobe nodule was detected in a 45-year-old woman who underwent a screening chest x-ray due to a history of smoking. Subsequent chest computed tomography (CT) showed a nodule with irregular margins and small peripheral foci of air at the inferior margin, possibly reflecting eccentric cavitation or underlying air bronchograms. Foci concerning for mucoid impaction were noted. A CT-guided fine needle aspiration and biopsy were subsequently performed.
Quiz:
Q1. Based on the images shown, which history is most likely for this patient?
- Owns a parrot
- Enjoys spelunking on weekends
- Recently moved to Fresno, California
- Endorses abuse of inhaled drugs
- Raises livestock for a living
Q2. Most people infected with this agent:
- Are asymptomatic, or have subclinical symptoms
- Experience a self-limiting pneumonia
- Develop a chronic infection
- Present with disseminated disease
Q3. True or False. If this organism is suspected, the laboratory should be alerted, as it is highly infectious and has the ability of grow on routine culture media.
Answers to Quiz
Q2. A
Q3. True
Diagnosis
Discussion
Coccidioides immitis is a dimorphic fungus native to hot, dry regions of the Southwestern United States, Central and South America. In a host, Coccidiodes take on their yeast form, the spherule, which is a large (15-100 µm) sphere containing between 800 and 1,000 endospores (1-5 µm) when mature. Upon rupture, these endospores are released into tissue, and may form new spherules. In the environment Coccidiodes form septate hyphae composed of thick walled, barrel shaped arthroconida which form along the hyphae alternating with brittle, thin walled abortive arthroconidia allowing for easy release of infectious spores.
Our case is unusual in that saprophytic hyphal forms are present in the body. This phenomenon, while possibly underrecognized in clinical practice, has been documented in the literature. Muñoz et al. report the presence of hyphal forms in 15 of 26 tissue or cytology specimens from culture confirmed coccidioidomycosis in Mexico, where the fungus is endemic. From a diagnostic perspective, it is important that pathologists are aware that hyphae may be seen in surgical pathology and cytology specimens so that Coccidioides is not overlooked as a potential etiologic agent due to the presence of hyphae. Additionally, finding the infectious form of the fungus in tissue theoretically raises a concern for person to person spread of infection, but this has not been documented to our knowledge.
Due to the extremely infectious nature of the arthroconidia of Coccidiodes, it considered an agent of bioterrorism by the federal government. When infection by Coccidiodes is suspected in clinical practice, it is imperative to inform the clinical laboratory, particularly in non-endemic areas. Biosafety level 2 practices are indicated for culture of this organism, and its ability to grow on routine culture media on the benchtop poses a potential danger to laboratory staff.
In endemic areas, infection is common. A positive skin test is observed in 50-90% of residents of endemic areas. The majority of infections are subclinical. Of those who develop clinically significant infections, approximately one half to two thirds will develop a self-limited pneumonia. The onset of symptoms is one to three weeks following inhalation of arthroconidia. The constellation of symptoms known as “Valley Fever” is named after the San Joaquin River Valley in California where Coccidioides immitis is endemic. Valley Fever is characterized by malaise, cough, chest pain, fever, and arthralgia. The course is generally self-limiting, with resolution of symptoms typically within two to six weeks. About 5-10% of patients can progress to a chronic pulmonary infection with cavity formation. Chronic infections may have a slowly progressive clinical course. Less than 1% of cases disseminate to other parts of the body. However, in heavily immunosuppressed patients, the rate of disseminated disease can be as high as 30-50%. For reasons that are not well understood, disseminated infection is more common in patients of African of Filipino ancestry. Coccidioidal meningitis is particularly concerning and requires lifelong antifungal treatment.
Infection confers immunity to a second primary infection in nearly all patients infected via CD4-related immunity. IgM antibodies may be detectable in a large percentage of newly infected individuals within three weeks after infection, with IgG following three weeks or later. IgG disappears after resolution of infection. In disseminated disease, IgG titer is proportional to severity of disease and indicative of prognosis.
Treatment with antifungal therapies is generally not indicated since the majority of infections are self limited. However, to reduce the risk of dissemination in immunocompromised patients or to treat patients with severe pneumonia, Itraconazole is the antifungal treatment of choice. Fluconazole can be considered as an alternative antifungal therapy, particularly for CNS infections due to its increased CSF penetration. In cases of rapidly progressive disseminated illness, respiratory failure, or pregnancy, amphotericin B may be indicated.
Take home message for trainees: Be aware that Coccidioides immitis infection may show saprophytic hyphal forms in addition to the classic endospores with spherules.
References
The Systemic Fungal Pathogens: Cryptococcus, Histoplasma, Blastomyces, Coccidioides, Paracoccidioides. In: Ryan KJ. eds. Sherris Medical Microbiology. 7th ed. New York, NY: McGraw-Hill. http://accessmedicine.mhmedical.com/content.aspx?bookid=2268§ionid=176088686. Accessed October 24, 2018.
Saubolle MS, McKellar PP and Sussland D. Epidemiologic, Clinical and Diagnostic Aspects of Coccidioidomycosis. J Clin Microbiol.2007;45:26-30.
Galgiani JM, et al. Coccidioidomycosis. Infectious Disease Society of America Practice Guidelines. Clinical Infectious Diseases. 2005;41:1217-23.
Munez B, et al. Parasite Mycelial Forms of Coccidioides Species in Mexican Patients. J Clin Microbiol. 2004;42:1247-49.
Meyer PR, Hui AN and Biddle M. Coccidioides immitis meningitis with arthroconidia in cerebrospinal fluid: report of the first case and review of the arthroconidia literature. Hum. Pathol. 1982;13:1136-38.
Nosanchuk JD, Snedeker J and Nosanchuk JS. Arthroconidia in coccidioidoma: case report and literature review. I J Infect Dis. 1998;3:32-35.
Contributor
Memorial Sloan Kettering Cancer Center
New York, NY, USA