Click here to see all images
February, 2018
Case of the Month
Clinical History:A 39-year-old woman with a past medical history of asthma since childhood and no previous smoking history or exposure acutely developed severe bronchial obstruction and eosinophilia. (Figures 1-6).
Quiz:
Q1. The predominant cells in the sections are:
- Lymphocytes
- Eosinophils and lymphocytes
- Neutrophils
- Histiocytes
- Langerhans cells
Q2. What would be most unlikely radiologic manifestations associated with these histological findings?
- Patchy consolidations
- Air entrapment
- Bilateral ground glass opacities
- Centrilobular emphysema
- Reticulonodular densities along lymphatics
Q3. Which of the following would not describe the findings seen in this case?
- Asthma
- Follicular bronchiolitis
- Pulmonary infiltrates
- Extravascular eosinophils
- Positive pANCA
Q4. Which of the following pathologies should be included in the differential diagnosis?
- Drug reaction
- Chronic hypersensitivity pneumonitis
- Diffuse alveolar damage
- Infection
- A and D
Answers to Quiz
Q2. E
Q3. B
Q4. E
Diagnosis
Discussion
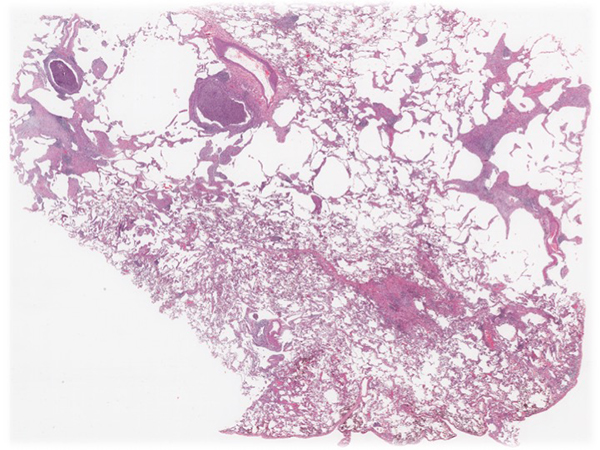
The natural clinical history comprises an early pre-vasculitic phase with overt allergic rhinitis, asthma (Figures 1 shows obstructive features comprising cellular bronchiolitis and luminal mucous plugs and figure 2 demonstrates classic features of asthma including moderate inflammation in the lamina propria and marked goblet cell hyperplasia), and blood and tissue eosinophilia, but no vasculitis clinically or in the biopsy; the vasculitic phase with eosinophilic-rich necrotizing or non-necrotizing vasculitis involving primarily small arteries (Figure 3 demonstrates necrotizing granulomatous vasculitis in small arteries), veins (Figure 4 shows venulitis) and capillaries (Figure 5 demonstrates capillaritis), granulomas and eosinophilic tissue infiltration (Figure 6). All these classic findings are not always actually found in the biopsy, particularly if the patient has been previously treated. In the postvasculitic phase in successfully treated patients the biopsy may show non-specific changes such as thrombosed small vessels in vessels with loss of the elastic layer.
The differential diagnosis of EGPA in the lung consists of diseases with tissue eosinophilia such as chronic eosinophilic pneumonia, allergic bronchopulmonary aspergillosis, parasitic infections, drug reactions, hypereosinophilic syndrome, and occasionally a fungal or tuberculosis infection. Other forms of ANCA-positive vasculitis such as microscopic polyangiitis and granulomatosis and polyangiitis (GPA, formerly Wegener’s granulomatosis) may also fall into the differential.
Our patient presented with asthma since childhood, developed pulmonary infiltrates, had blood eosinophilia (46%), and was found to have an increased p-ANCA. Following the diagnostic criteria of the American College of Rheumatology, the patient was subsequently diagnosed as EGPA.
Take home message for trainees: EGPA is an pANCA-associated vasculitis characterized by eosinophilic tissue infiltration, necrotizing or non-necrotizing vasculitis and granulomas seen in a patient with a history of asthma, allergic rhinitis, pulmonary infiltrates, mono/polyneuropathy and marked blood eosinophilia. Do not diagnosis EGPA in the absence of asthma and blood eosinophilia.
References
Masi T, Hunder GG, Lie TT et al. The American College of Rheumatology. 1990 criteria for the classification of Churg Strauss Syndrome. Arthritis Rheum. 1990, 33:1094-100.
Calatroni M, Oliva E, Gianfreda D et al. ANCA-associated vasculitis in childhood: recent advances. Italian Journal of Pediatrics. 2017; 43:46.
Contributors
Histopathology Department
Manchester University Hospitals
Wythenshawe Hospital
Manchester, UK