Click here to see all images
January, 2018
Case of the Month
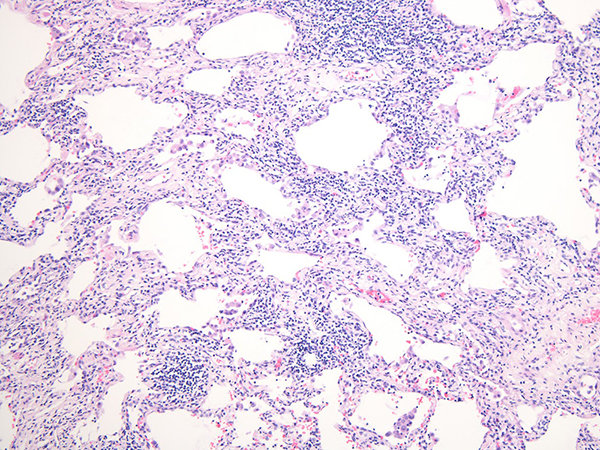
Clinical History:A 58-year old woman with past medical history of arthritis and psoriasis presented with progressive shortness of breath. Wedge biopsies of left upper and lower lobes are shown (Figures 1-6).
Quiz:
Q1. The predominant cells seen in the sections are:
- Histiocytes
- Lymphocytes
- Eosinophils
- Neutrophils
- Type II pneumocytes
Q2. What would be most likely radiologic manifestations associated with these histologic findings?
- Dense lobar consolidation
- Bilateral angiocentric cavitary nodules
- Reticular opacities with honeycomb changes mainly involving lower lobes
- Tiny reticulonodular densities along the lymphatic
- Bilateral ground glass opacities
Q3. The most feasible clinical scenario that could be expected in this case:
- Live with pet birds in a moldy house
- Long standing rheumatoid arthritis
- Heavy occupational exposure to asbestos
- Recent respiratory failure due to exposure to toxic fumes
- Current heavy smoker with severe COPD
Q4. Which of the following would not describe the findings seen in this case?
- Peribronchial lymphoid follicles with prominent germinal centers
- Preserved alveolar architecture without honeycomb changes
- Nonspecific lymphoid aggregates in the peribronchial stroma and alveolar septa
- Numerous fibroblast foci
- Diffuse interstitial lymphocytic infiltrates
Answers to Quiz
Q2. E
Q3. B
Q4. D
Diagnosis
Discussion
NSIP can be categorized as either cellular, fibrotic, or as a mixed cellular and fibrotic pattern. Cellular NSIP is characterized by interstitial lymphocytic and plasma cell infiltrates without significant fibrosis. Variable degrees of fibrosis can be present in fibrotic NSIP, which can be subclassified as mixed cellular and fibrotic or fibrotic NSIP depending on the degree of fibrosis. A uniform pattern of interstitial inflammation, as seen in this case, is characteristic for cellular NSIP (Figures 1 and 2). Fibrotic NSIP also shows a uniform pattern of distribution of fibrosis as opposed to the patchwork of fibrosis seen in UIP. Moreover, fibrotic NSIP shows temporally uniform chronic fibrosis with collagen deposition, in contrast to the temporal heterogeneity of fibrosis in UIP characterized by chronic fibrosis juxtaposed with more active fibrosis as shown by fibroblast foci. Lymphoid follicles with prominent germinal centers around bronchioles are diagnostic for follicular bronchiolitis (Figures 3 and 6), which tend to result in obstructive pulmonary function abnormalities, likely due to compression of the bronchiolar lumens by enlarged lymphoid follicles.
NSIP can be idiopathic or associated with underlying conditions, including connective tissue disease, hypersenstitivity pneumonitis (HP), drug reaction, and infection, among others. The presence of follicular bronchiolitis as well as NSIP in this case favors an underlying connective tissue disease such as rheumatoid arthritis, although one cannot completely exclude a possibility of HP. Absence of granulomas or organizing pneumonia would argue against the diagnosis of HP. A possibility of drug reaction or infection should be excluded by a careful clinical evaluation as well.
The most common presenting symptoms of NSIP are dyspnea and cough. Fever and constitutional symptoms may also occur. The average age of idiopathic NSIP patients is in 50’s, a decade younger than that of idiopathic UIP patients, with a female predominance. High resolution computed tomography (HRCT) most commonly shows bilateral ground glass opacities with irregular reticular densities and occasional traction bronchiectasis in the majority of cases. Honeycomb changes are usually absent in NSIP on HRCT; however, some NSIP cases might show subpleural reticular densities and minor areas of honeycomb changes, which makes it very difficult to distinguish from UIP on HRCT. Biopsy is then needed to reach a definite diagnosis in such cases. The prognosis of NSIP is generally favorable, though somewhat variable.
Take home message for trainees: Connective tissue diseases may present as interstitial lung disease, most commonly as NSIP and are often accompanied by follicular bronchiolitis, especially in rheumatoid arthritis.
References
Belloli EA, Beckford R, Hadley R, et al. Idiopathic non-specific interstitial pneumonia. Respirology. 2016 Feb; 21(2):259-68.
Kadoch MA, Cham MD, Beasley MB, et al. Idiopathic interstitial pneumonias: a radiology-pathology correlation based on the revised 2013 American Thoracic Society-European Respiratory Society classification system. Curr Probl Diagn Radiol. 2015 Jan-Feb; 44(1):15-25.
Tansey D, Wells AU, Colby TV, et al. Variations in histological patterns of interstitial pneumonia between connective tissue disorders and their relationship to prognosis. Histopathology. 2004 Jun; 44(6):585-96.
Contributors
(Joanne) Eunhee S. Yi, M.D. Professor Department of Laboratory Medicine and Pathology Mayo Clinic, Rochester, MN, USA.