Click here to see all images
May, 2018
Case of the Month
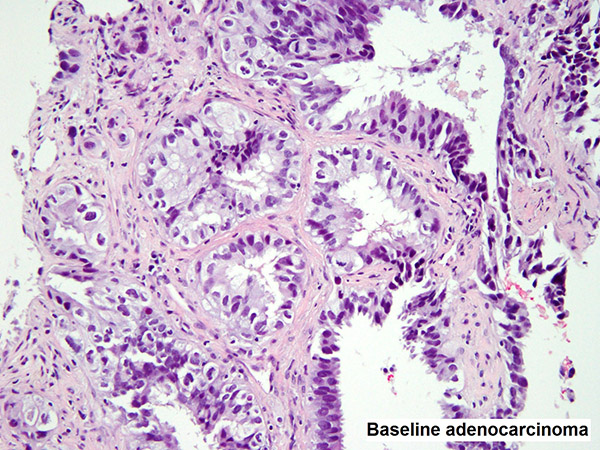
Clinical History:A 57-year-old woman with stage IV lung adenocarcinoma (Figure 1) with an EGFR L858R mutation was treated with erlotinib (an EGFR tyrosine kinase inhibitor). After initial response to treatment for over 1 year, she developed extensive metastatic disease at the T5 vertebra (biopsy shown in Figure 2). By immunohistochemistry, the tumor labeled for CAM 5.2, TTF-1, synaptophysin, and chromogranin A (Figure 3). The Ki-67 (MIB-1) labeling index was over 70% (Figure 4).
Quiz:
Q1. What is the histologic diagnosis for figure 2?
- Squamous cell carcinoma
- Small cell carcinoma
- Adenocarcinoma
- Adenosquamous carcinoma
Q2. Which of the following is an acquired resistance mechanism to therapy with EGFR tyrosine kinase inhibitors in lung adenocarcinoma?
- EGFR exon 20 T790M mutation
- MET amplification
- Small cell transformation
- All of the above
Q3. Small cell transformation constitutes what percentage of all acquired resistance mechanisms in lung adenocarcinomas treated with EGFR tyrosine kinase inhibitors?
- 85-95%
- 50-85%
- 15-50%
- 5-15%
Answers to Quiz
Q2. D
Q3. D
Diagnosis
Discussion
For patients receiving EGFR inhibitors, after initial tumor response to treatment, relapse and disease progression inevitably occur due to acquired resistance to targeted therapy. The median time to development of acquired resistance is 1 year, but can be many years. The most common mechanism of resistance is the acquisition of a secondary EGFR exon 20 T790M mutation. In addition, transformation of EGFR-mutated lung adenocarcinomas to small cell carcinoma is well established as a resistance mechanism in a minority of patients (5-15%). Disease progression from the primary lung adenocarcinoma has been supported by the fact that, in these cases, small cell carcinomas harbor the initial EGFR activating mutation; a finding not found in de novo small cell carcinomas.
The morphology of small cell carcinoma in acquired resistance samples is identical to that of de novo small cell carcinoma. It is characterized by densely packed sheets of small tumor cells with finely granular chromatin and absent to inconspicuous nucleoli. Nuclear molding, necrosis, and a high mitotic index are typical features. The diagnosis can be supported by labeling for neuroendocrine markers (chromogranin A, synaptophysin, CD56, and the recent marker INSM1). TTF-1 is positive in over 90% of cases. The Ki-67 (MIB-1) labeling index is high (50-100%). Small cell histology is not found in pre-treatment samples, which show conventional adenocarcinoma morphology (as seen in Figure 1).
Finally, while small cell transformation is not a new concept and has been seen in other tumors of various organ systems (e.g. prostatic adenocarcinoma after androgen deprivation therapy), small cell transformation of lung adenocarcinomas is no longer solely seen in EGFR-mutated cases. ALK-rearranged lung adenocarcinomas have now been found to transform to small cell carcinoma as a resistance mechanism under the selective pressure of ALK inhibitor therapy.
Lastly, it is worth noting that acquired resistence to first and second generation EGFR inhibitors –erlotinib and afatinib, respectively, is well described and is known to be associated with small cell transformation. However, a third generation EGFR inhibitor osimertinib has recently been introduced as first-line treatment for EGFR mutant lung carcinomas. Mechanisms of resistance in this setting remain to be described.
Take home message for trainees: Small cell transformation is one of several acquired resistance mechanisms in lung adenocarcinomas with sensitizing EGFR mutations that are treated with first and second generation EGFR inhibitors. Recognition of small cell carcinoma transformation in acquired resistance samples is critical as this requires a switch to small cell-directed chemotherapy regimens.
References
Levacq D, D'Haene N, de Wind R, et al. Histological transformation of ALK rearranged adenocarcinoma into small cell lung cancer: A new mechanism of resistance to ALK inhibitors. Lung Cancer 2016;102:38-41.
Sequist LV, Waltman BA, Dias-Santagata D et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med 2011;3:75ra26.
Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med 2018;378:113-25.
Yu HA, Arcila ME, Rekhtman N, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR TKI therapy in 155 patients with EGFR mutant lung cancers. Clin Cancer Res 2013;19:2240-7.
Contributors
Oncologic Surgical Pathology Fellow
Department of Pathology
Memorial Sloan Kettering Cancer Center (MSKCC), New York, NY, USA
Natasha Rekhtman, M.D., Ph.D.
Associate Attending Pathologist
Thoracic Pathology and Cytopathology
Department of Pathology
Memorial Sloan Kettering Cancer Center (MSKCC), New York, NY, USA