Click here to see all images
November, 2018
Case of the Month
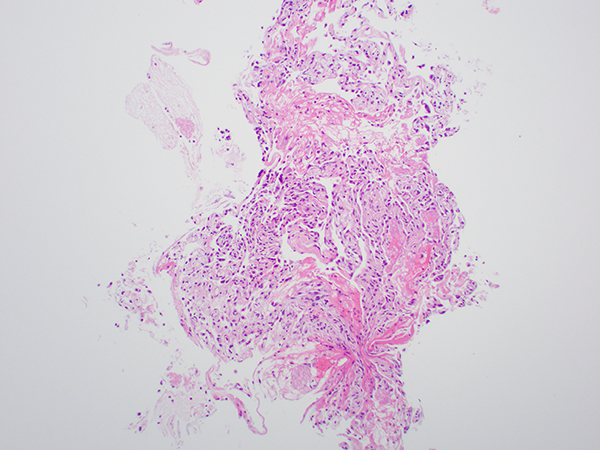
Clinical History: A 35-year-old man with a history of smoking and HIV infection presents with dry cough, fever with sweats, and difficulty in breathing for several days. Clinical examination reveals an increased respiratory rate, tachycardia, and fine crackles on auscultation of the chest. Chest radiograph shows diffuse bilateral infiltrates and subsequent high resolution computed tomography shows multiple ground glass opacities in the lung. Bronchoalveolar lavage (BAL) and transbronchial biopsy (Figure 1-3) are performed. Tissue is also sent for bacterial, fungal and mycobacterial cultures
Quiz:
Q1. Which of the following techniques is currently the preferred definitive diagnostic tool for Pneumocystis jirovecii pneumonia (PJP)?
- Detection of cysts and/or trophic forms by special stains
- Elevated lactate dehydrogenase (LDH)
- Polymerase chain reaction
- β-D-Glucan detection
Q2. Which of the following risk factors is most commonly associated with Pneumocystis jiroveci/carinii pneumonia?
- Exposure to broad spectrum antibiotics
- Human Immunodeficiency virus (HIV) infection
- Prior history of leukemia/lymphoma
- Smoking
Q3. Which of the following infectious organisms is most likely to be considered in the differential diagnosis of PJP when examining GMS stains?
- Aspergillus
- Histoplasma
- Mycobacteria
- Nocardia
Answers to Quiz
Q2. B
Q3. B
Diagnosis
Discussion
Primary exposure to Pneumocystis occurs early in life; organisms remain in the latent form and are reactivated in an immunocompromised host. Four developmental forms of Pneumocystis are described: trophozoites, precysts, sporozoites, and mature cysts. Through cell wall thickening, the trophozoites develop into precysts, and then, through meiosis and mitosis, sporozoites are formed. Mature cysts contain multiple sporozoites. The cysts are the forms can be seen in tissue sections, are 5-7 µm in size, and are round-to-oval, crescent-shaped, disk-shaped, or boat-shaped organisms identified readily by GMS and PAS stains. The typical features of pneumocystis pneumonia consist of chronic interstitial inflammation and frothy eosinophilic exudates. Rarely, pneumocystis pneumonia presents as granulomatous inflammation in patients who are marginally immunocompromised. Granulomas are loose to well-formed and can be with or without necrosis.
Bronchoalveolar lavage (BAL) and induced sputum samples are frequently used for the detection of PCP/PJP. Definitive diagnosis requires identification of the fungi by routine cytological staining techniques (Giemsa, Papanicolaou, and GMS) or direct fluorescent antibody staining on these samples. IHC and polymerase chain reaction (PCR) are also used with slightly more promising results; however, these techniques are laborious, costly, and therefore less commonly used. An elevated lactate dehydrogenase (LDH) is often used as a clinical indicator of possible PCP in HIV-infected individuals; however, LDH can be elevated from underlying hematologic malignancies or other causes. β -D-glucan is a cell wall component of most fungi, including Pneumocystis, and can be elevated in the setting of a number of other fungal infections.
Antimicrobial therapy directed against P. jirovecii (trimethoprim-sulfamethoxazole) is the mainstay of treatment. In addition, some patients require adjunctive corticosteroids. Most patients have excellent prognosis on therapy with fatality of less than 10% in patients with mild to moderate disease and more than 20% in patients with severe disease.
Take home message for trainees: Although PCR is highly sensitive, transbronchial lung biopsy remains the cornerstone for confirmation of Pneumocytis pneumonia.
References
Jacobs JA, Dieleman MM, Cornelissen EI, et al. Bronchoalveolar lavage fluid cytology in patients with Pneumocystis carinii pneumonia. Acta Cytol 2001;45:317.
Wazir JF, Ansari NA. Pneumocystis carinii infection. Arch Pathol Lab Med 2004; 128:1023-7.
Contributor
Kaiser Permanente Medical Center, Santa Clara
700 Lawrence Expressway, Department 204
Santa Clara, CA 95051