Click here to see all images
January, 2019
Case of the Month
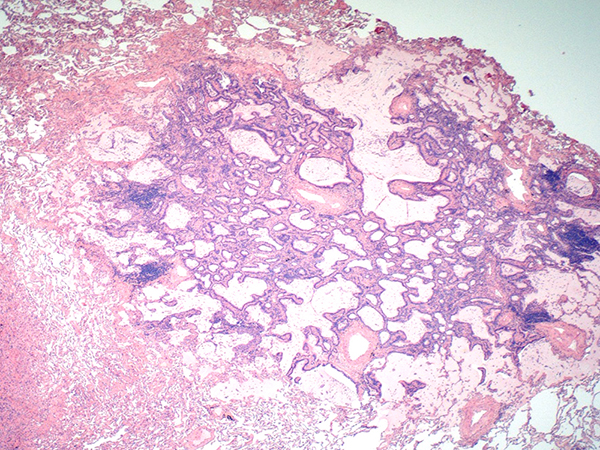
Clinical History: A 75 year old female with a history of a previously resected right upper lobe pulmonary adenocarcinoma presented with two nodules in the left upper lobe 14 years later. The patient underwent a left upper lobe wedge resection encompassing both radiographic nodules. Grossly, distinct 10.0 mm and 4.0 mm nodules were identified. The larger nodule was a classical non-mucinous acinar predominant adenocarcinoma; however, the smaller nodule had a different appearance, as illustrated in Figures 1-6.
Quiz:
Q1. Which of the following is true about the expected behavior of this lesion?
- Aggressive behavior with early metastases
- Locally aggressive spread, ultimately producing a “pneumonic” type consolidation of the lung
- Indolent behavior, putatively benign
- Highly likely to recur after resection
Q2. Which is the following is true about this lesion?
- It is a variant of mucinous adenocarcinoma
- It is a type of peribronchiolar metaplasia
- It is a variant of mucoepidermoid carcinoma
- It is postulated to be part of a spectrum of bronchial adenomas
Q3. Which is the following is true about this lesion?
- It does not have known genetic abnormalities
- It is characterized by an EWSR1-CREB1 fusion
- It has most frequently shown mutations in BRAF, but mutations in EGFR, KRAS and other driver genes have been reported.
- It classically has a SMARCB1 or SMARCA4 deficiency
Answers to Quiz
Q2. D
Q3. C
Diagnosis
Discussion
Take home message for trainees: CMPT is a rare but increasingly recognized neoplasm of the lung which may be easily mistaken for mucinous adenocarcinoma. The bi-layered tumor morphology consisting of ciliated and mucinous cells overlying a uniform row of basal cells is a unique feature of CMPT which should aid in identification.
References
Ishikawa, Y., Ciliated muconodular papillary tumor of the peripheral lung: benign or malignant. Pathol Clin Med (Byouri-to-Rinsho) 2002; 20: 964-965.
Kamata, T.; Yoshida, A.; Kosuge, T, et al. Ciliated muconodular papillary tumors of the lung: a clinicopathologic analysis of 10 cases. Am J Surg Path 2015; 39: 753-60.
Kamata, T.; Sunami, K.; Yoshida, A., et al. Frequent BRAF or EGFR Mutations in ciliated muconodular papillary tumors of the lung. J Thor Onc 2016; 11: 261-5.
Kon, T.; Baba, Y.; Fukai, I., et al. Ciliated muconodular papillary tumor of the lung: A report of five cases. Pathol Intl 2016; 66: 633-639.
Contributors
Shahram Saberi, MD and Mary Beth Beasley, MD
Department of Pathology
Icahn School of Medicine at Mount Sinai
1 Gustave L. Levy Pl
New York, NY 10029
USA