Click here to see frozen section images 1 & 2
March, 2019
Case of the Month
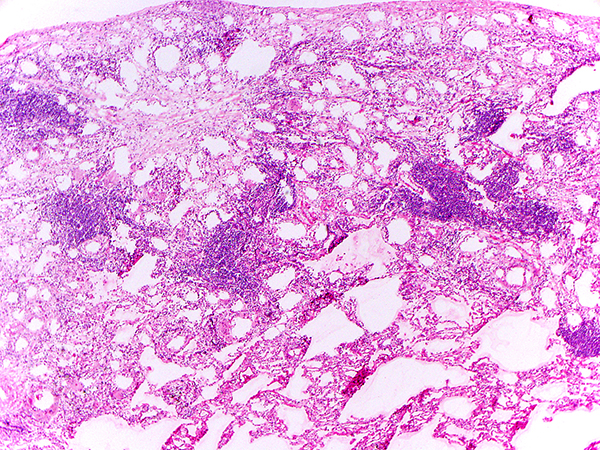
Clinical History:A 85-year-old female former smoker with a history of thyroid and breast cancer presented with a 10-cm right-sided lower lobe pleural-based mass and a separate 2-cm triangular opacity in the dependent aspect of the right middle lobe of lung along the major fissure. CT-guided biopsy of the 10-cm mass demonstrated a solitary fibrous tumor. The patient underwent resection of the right lower lobe mass and wedge resection of the right middle lobe lesion. An intraoperative frozen section of the 2-cm right middle lobe lesion is shown in Figures 1-2.
Quiz:
Q1. During intraoperative consultation, in review of Figures 1-2, which of the following is the appropriate interpretation for this 2-cm lesion:
- Metastatic solitary fibrous tumor
- Adenocarcinoma, acinar predominant
- Granulomatous infection, possibly cryptococcal pneumonia
- Multinucleated giant cells and lymphoid aggregates; no evidence of carcinoma/sarcoma
- Multiple lymphoid aggregates, most consistent with low grade B-cell lymphoma
Case continued....
Representative images of the 2-cm lesion on permanent are shown in Figures 3-5 (click here for permanent section images 3-5)
Q2. After reviewing Figures 3-5, which of the following is true about this 2-cm lesion?
- It is characterized by NAB2-STAT6 gene fusion.
- It is characterized by IGH gene rearrangement.
- It may harbor BRAF V600E mutation.
- It exhibits GMS-positive yeast forms; mucicarmine stain may be negative, but Fontana-Masson stain usually demonstrates melanin precursors within the cell wall of the yeasts.
- It is not neoplastic or infectious disease.
Q3. After reviewing Figures 3-5, which of the following is true about this 2-cm lesion?
- Prognosis would depend on whether it harbors TERT promoter mutation.
- It is associated with pulmonary involvement by collagen vascular disease.
- Exposure such as use of mineral oil should be inquired.
- The patient’s immunosuppressive condition has played a significant role.
- Bilateral cortical sclerosis of long bones is characteristic.
Answers to Quiz
Q2. E
Q3. C
Diagnosis
Discussion
Given its distinctive morphology, differential diagnosis for exogenous lipoid pneumonia is relatively narrow. Once one recognizes its reactive nature with its characteristic lipid vacuoles, other histiocytic disorders such as Rosai-Dorfman disease and Erdheim-Chester disease can be excluded. Endogenous lipoid pneumonia, in which the accumulated lipid is derived from intrinsic metabolism rather than exogenous source, may be considered, though the cytoplasm of the histiocytes is often more foamy (microvesicular) lacking conspicuous large vacuoles, and it is often associated with bronchial obstruction rather than exogenous lipid use. Of note, during intraoperative consultation for a lung mass/nodule, exogeneous lipoid pneumonia may be confused with granulomatous infection due to the combination of inflammation and giant cell reaction. If vacant holes associated with giant cells are recognized and the possibility of lipid vacuoles are considered, Oil Red O stain (or other lipid stains) would help confirming the diagnosis. While the clinical course of exogenous lipoid pneumonia may be variable, depending on its extent and distribution and the patient’s constitution, once the use of the offending agent ceases, it is generally benign.
References
Franquet T, Giménez A, Bordes R, et al. The crazy-paving pattern in exogenous lipoid pneumonia: CT-pathologic correlation. AJR Am J Roentgenol 1998;170:315-7.
Laurent F, Philippe JC, Vergier B, et al. Exogenous lipoid pneumonia: HRCT, MR, and pathologic findings. Eur Radiol 1999;9:1190-6. Marchiori E, Zanetti G, Mano CM, et al. Exogenous lipoid pneumonia. Clinical and radiological manifestations. Respir Med 2011;105:659-66.
Wang CW, Colby TV. Histiocytic lesions and proliferations in the lung. Semin Diagn Pathol 2007;24:162-82.
Contributors
Department of Pathology
Massachusetts General Hospital
55 Fruit Street
Boston, MA 02114
USA