Click here to see all images
February, 2020
Case of the Month
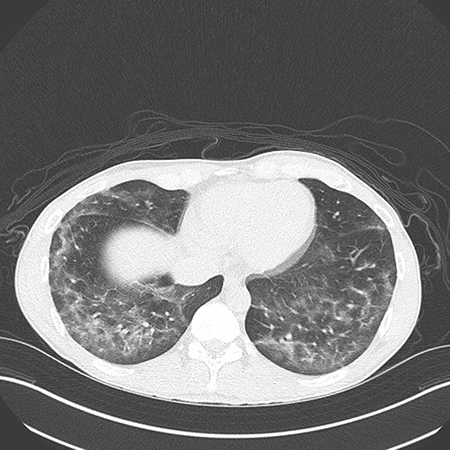
Clinical History: A young man in his 20s presented with fever, nausea, dyspnea and dry cough for 5 days. On examination, he was febrile and hypoxic on room air. Chest CT showed bilateral ground-glass opacities with areas of consolidation and some degree of subpleural sparing (Figure 1). Laboratory work-up showed leukocytosis, elevated ESR and elevated C-reactive protein. The patient was well prior to onset of these symptoms, with no significant chronic medical issues. There was no history of HIV/AIDS or other immunosuppression. The patient “smoked weed” daily and also vaped tetrahydrocannabinol (THC) frequently, the last episode being 7 days prior to onset of his symptoms. He was initially treated for presumed pneumonia but after a lack of response to treatment (and negative serologies and cultures), bronchoscopy with bronchoalveolar lavage (BAL) and transbronchial lung biopsies was performed. The BAL fluid revealed predominantly macrophages (Figure 2) without large or coarse vacuoles. Cultures of the BAL fluid were negative. Images from the transbronchial lung biopsy are shown in Figures 3-6.
Quiz:
Q1. Which of the following is true regarding this patient?
- The lung biopsy shows acute lipoid pneumonia, confirming the diagnosis of vaping-related lung injury
- An oil red O test is mandatory to confirm the diagnosis
- The lung biopsy shows acute lung injury
- Vaping is known to be safe and cannot explain these symptoms
Q2. Which of the following is true regarding the oil red O stain in bronchoalveolar lavage fluid?
- A negative oil red O stain excludes vaping-related lung injury
- A positive oil red O stain is specific for vaping-related lung injury
- Oil red O staining is diagnostic of exogenous lipoid pneumonia
- Oil red O staining is not required for the diagnosis of vaping-related lung injury
Q3. Which of the following is true regarding lung biopsies from patients with vaping-related lung injury?
- The diagnosis of acute lipoid pneumonia has been confirmed by lung biopsies from these patients
- Two lung biopsy series published during the outbreak have reported acute lung injury patterns
- Exogenous lipoid pneumonia cannot be diagnosed by lung biopsies because lipid is removed during processing
- Foamy macrophages are indicative of lung damage caused by an inhaled lipid-containing substance
Answers to Quiz
Q2. D
Q3. B
Diagnosis
Clinical diagnosis: Vaping-associated acute lung injury
Discussion
“Vaping” is the inhalation of an aerosol generated by heating a liquid in a handheld battery-powered device. The liquid is generally contained in a cartridge. Although the variety of vaping devices, cartridges and terminologies is highly complicated, there are two broad categories. The first consists of store-bought e-cigarettes that produce a nicotine-containing aerosol. The second consists of devices that use THC-containing cartridges purchased mostly from illicit sources. In mid-2019, several reports appeared of a sudden outbreak of cases of acute respiratory illness in individuals who reported vaping prior to the onset of their symptoms. This outbreak peaked in September 2019; the number of reported cases is currently declining. During the investigation of the outbreak, the Centers for Disease Control and Prevention (CDC) termed this entity “E-cigarette, or Vaping, Product Use-Associated Lung Injury (EVALI)”. At the time of this writing (January 2020), 2,668 hospitalized cases of EVALI have been reported. Per the CDC, median patient age is 24 years, and 66% of patients are male. Importantly, the majority of cases in the EVALI outbreak have been linked to the use of THC-containing cartridges purchased in an illicit fashion. Per CDC data, 82% of patients report using a THC-containing vaping product, whereas 14% report using only nicotine-containing products. It is now believed that the illegal “cutting” (dilution) of THC oils with vitamin E acetate may be responsible for the lung injury in these patients. One hypothesis is that the heating of vitamin E acetate may lead to the formation of toxic byproducts that cause lung damage when inhaled.
The lung biopsy in the current case does not show “acute lipoid pneumonia”. It shows acute lung injury along with a few non-specific foamy macrophages. Exogenous lipoid pneumonia, a well-known clinicopathologic entity, is characterized by macrophages with large, coarse vacuoles and multiple empty spaces within the interstitium (these spaces are caused by the removal of lipid from the section by processing) accompanied by multinucleated giant cells and varying degrees of fibrosis (for an example, see Case of the Month, March 2019). Despite the fact that some lipid is removed from biopsies by processing of formalin-fixed paraffin-embedded tissue, exogenous lipoid pneumonia has been diagnosed in lung biopsy and resection samples since 1925. This is because the spaces left behind by the dissolved lipid remain visible within the interstitium, accompanied by other valuable clues such as giant cells, fibrosis, and macrophages with large vacuoles. In contrast, foamy macrophages with small or indistinct vacuoles are exceedingly common in lung biopsies and resections in a variety of settings, the best known being post-obstructive changes (so-called “golden pneumonia”). These macrophages are a non-specific finding, and are thought to occur primarily due to phagocytosis of membrane lipid derived from the dead and degenerated cells within the lung. Since the lipid is “endogenous”, the unfortunate term “endogenous lipoid pneumonia” has become associated with this finding. As we have seen in the EVALI outbreak, this terminology has the potential to create immense confusion for pathologists, clinicians and the lay public.
Two lung biopsy series were reported during the EVALI outbreak; both showed acute lung injury patterns without evidence of exogenous lipoid pneumonia. Thus far, not a single biopsy-confirmed case of exogenous lipoid pneumonia has been reported in EVALI. Since there are no pathognomonic histologic features in EVALI, lung biopsies do not “confirm” the diagnosis; the diagnostic criteria are mainly clinical and radiologic. BAL and lung biopsies are not required in the majority of patients. When performed, their major utility is in excluding alternative etiologies such as infection. The oil red O stain has received much attention during this outbreak, but the pathology community (including lung pathologists and cytopathologists) have been quick to point out that this stain - notorious for being plagued with technical issues and difficulties in interpretation - is not specific for exogenous lipoid pneumonia (see Pambuccian et al and Saqi et al). A negative oil red O stain does not exclude the diagnosis of EVALI, and a positive oil red O test is not specific for EVALI. Therefore, the role of this stain in the diagnosis of EVALI is highly questionable.
Take home message for trainees: Lung biopsies from patients with vaping-associated lung illness show acute lung injury patterns, not “lipoid pneumonia”..
References
Larsen BT, Butt Y, Smith ML. More on the pathology of vaping-associated lung injury. N Engl J Med 2020;382:387-90.
Mukhopadhyay S, Mehrad M, Dammert P, et al. Lung biopsy findings in severe pulmonary illness associated with e-cigarette use (vaping). Am J Clin Pathol 2020;153:30-9.
Pambuccian SE. Testing for lipid-laden macrophages in bronchoalveolar lavage fluid to diagnose vaping-associated pulmonary injury. Are we there yet? J Am Soc Cytopathol 2020;9:1-8.
Saqi A, Mukhopadhyay S, Butt Y, et al. E-cigarette or vaping product use-associated lung injury: what is the role of cytologic assessment? Cancer Cytopathol 2020; Epub ahead of print
Contributor
Director, Pulmonary Pathology
Cleveland Clinic, Cleveland, OH