Click here to see all images
October, 2020
Case of the Month
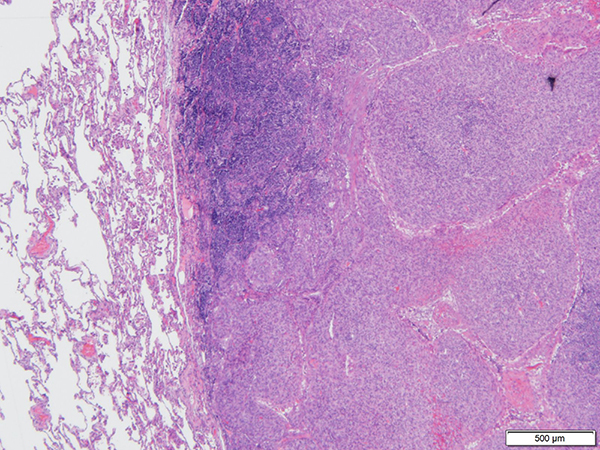
Clinical History: A 59-year-old man was found to have 1.5-cm heterogeneous, non-calcified lung nodule in the left lower lobe on a surveillance CT scan, a year after a right hemicolectomy for a malignant mesothelioma. The nodule was sampled by a transthoracic core needle biopsy and fine-needle aspiration. The biopsy and FNA showed a dense fibrous pseudocapsule surrounding nodules of histiocytoid cells arranged in sheets, whorls, and short fascicles with round normochromatic nuclei, inconspicuous nucleoli, and vacuolated cytoplasm with associated lymphoid aggregates around the nodules (Figures 1 to 6). The neoplastic cells were positive for CD68, focally positive for desmin, and negative for EMA, pancytokeratin, CD21 and calretinin. A diagnostic molecular test was performed.
Quiz:
Q1. What is the most common presentation of this neoplasm?
- Mediastinal mass
- Metastasis to the bone
- Retroperitoneal soft tissue mass
- Soft tissue neoplasm of the deep dermis
Q2. What is the most commonly described gene fusion detected in this tumor?
- EWSR1-ATF1 fusion
- EWSR1-CREB1 fusion
- FUS-ATF1 fusion
- FUS-ERG fusion
Q3. What other tumors are characterized by EWSR1-CREB1 fusion?
- Extraskeletal myxoid chondrosarcoma
- Primary pulmonary myxoid sarcoma, malignant gastrointestinal neuroectodermal tumor, and clear cell sarcoma
- Sclerosing epithelioid fibrosarcoma and low grade fibromyxoid sarcoma
- Soft tissue myoepithelial tumor and myxoid liposarcoma
Answers to Quiz
Q2. B
Q3. B
Diagnosis
Discussion
Grossly, pulmonary AFH is similar to those arising in the soft tissue and demonstrates a nodular, well-circumscribed, and hemorrhagic cut surface. These tumors can also be multi-cystic. The median size is around 2 cm. Microscopically, AFH is encapsulated, with a dense fibrous pseudocapsule and associated lymphoid aggregates (mixture of B- and T-lymphocytes) around nodules, and often hypercellular with bland histiocytoid cells. Most cases have large, round, blood-filled spaces associated with surrounding hemosiderin deposition in the center of the lesion; although approximately one-third of cases show completely solid histology without these above-mentioned cavities. The cells surrounding the cystic spaces are uniform with monomorphic spindle to ovoid cells and eosinophilic cytoplasm. Occasionally, mitotic activity and pleomorphism can be seen; however these features are not associated with a worse outcome. The stroma can be myxoid or sclerotic, mimicking the desmoplastic stroma of a carcinoma. The cytopathologic features of AFH include histiocytoid cells in sheet, clusters or individual cells admixed with eosinophilic mesenchymal fragments and lymphocytes in the background of blood. Lesional cells may have pleomorphism with abundant cytoplasm and prominent nucleoli.
AFH does not have a specific immunoprofile. The combination of clinical presentation, histologic features, immunoprofile and molecular studies usually lead the pathologist to the final diagnosis. The tumor is positive for desmin in 50% of cases (can be diffuse or focal), CD68 (variable), and may also be occasionally positive for SMA, calponin and h-caldesmon. Ki-67 proliferative index is usually low (2-4%). Skeletal muscle immunostains like myogenin or MyoD1 have been consistently reported negative and are helpful in differentiating AFH from rhabdomyosarcoma. The tumor cells are also reported to be negative for endothelial markers including CD31, CD34, and factor VIII, as well as markers for S100 protein, cytokeratin, and lysozyme.
These tumors are characterized by rearrangements involving the EWSR1 or FUS genes with ATF1 or CREB1.The most common gene fusion is EWSR1-CREB1 t(2:22)(q33:q12), reported in more than 90% of the cases. Other gene rearrangements that have been reported in these tumors include t(12:22)(q13:q12) involving EWSR1-ATF1 and t(12:16)(q13:p11) involving FUS-ATF1. The EWSR1-ATF1 gene fusion has been reported to be more common in extrasomatic soft tissue cases of AFH such as primary pulmonary AFH. EWSR1-CREB1 fusions have been also been identified in malignant gastrointestinal neuroectodermal tumor, clear cell sarcoma of soft tissue, and primary pulmonary myxoid sarcoma.
There is long list of differential diagnoses for primary pulmonary AFH and it is important to have a high index of suspicion for pathologists to recognize this entity. Most cases can be diagnosed by a combination of immunohistochemistry and molecular testing for EWSR1 or FUS genes. Malignant melanoma can mimic AFH in lung and thus utilizing appropriate immunostains (such as SOX10, HMB45, Melan A) to rule out melanoma is crucial. Follicular dendritic cell sarcoma is another entity that has similar histological features to AFH, though the tumors cells in this entity are positive for CD21, CD23, and CD35. Kaposi sarcoma can be differentiated from AFH using HHV8 and endothelial markers such as CD31 and CD34. Other vascular tumors such as spindle cell hemangioma are also positive for CD31 and CD34. Pneumocytoma can be excluded using TTF1, which is positive in both surface and round cell components. Nodular fasciitis is generally negative for desmin and harbors the MYH9-USP6 gene fusion. And finally, undifferentiated pleomorphic sarcomas that tend to have marked nuclear atypia and occurs primarily in older individuals.
Take home message for trainees: AFH is a rare cytologically bland neoplasm of intermediate biologic potential that lacks distinguishing immunomarkers and is characterized by characteristic translocations involving the EWSR1 or FUS genes with ATF1 or CREB1.
References
Tay CK, Koh MS, Takano A, Aubry MC, Sukov WR, Folpe AL. Primary angiomatoid fibrous histiocytoma of the lung with mediastinal lymph node metastasis. Human pathology. 2016;58:134-7.
Thway K, Fisher C. Angiomatoid fibrous histiocytoma: the current status of pathology and genetics. Archives of Pathology and Laboratory Medicine. 2015;139(5):674-82.
Contributors
Cytopathology fellow
Department of Pathology
Division of Pathology/Lab Medicine
The University of Texas MD Anderson Cancer Center
Houston, TX, USA
Sinchita Roy-Chowdhuri, MD PhD
Associate Professor
Department of Pathology
Division of Pathology/Lab Medicine
The University of Texas MD Anderson Cancer Center
Houston, TX, USA