Click here to see all images
December, 2021
Case of the Month
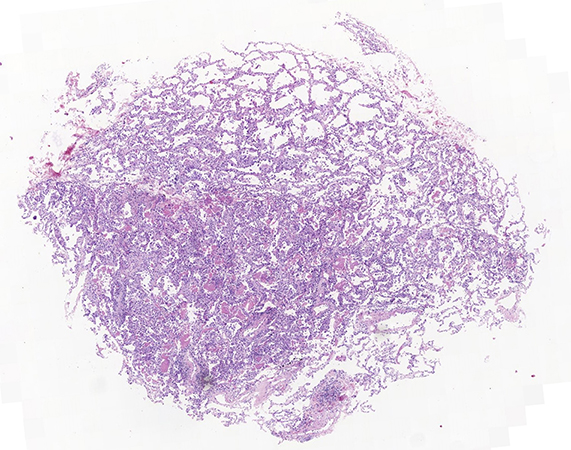
Clinical History: A 38-year-old man presented with progressive dyspnea. He was a sporadic smoker, who reported no significant past medical history. He worked in a shop, and had a parrot for more than 10 years. Three months prior to presentation, he developed dyspnea and was diagnosed with asthma, for which he began treatment, with clinical improvement. Two weeks prior to presentation, he complained of progressive dyspnea without wheezing associated with dry cough, and used bronchodilators again, this time without improvement. He also developed intermittent fever of up to 38ºC and sweating. A chest CT showed bilateral basal peripheral reticular opacities; which was interpreted as “cannot rule out interstitial pathology”. Five transbronchial cryobiopsies of different segments of the left lower lobe were performed, with a clinical differential diagnosis of “interstitial pneumopathy vs. atypical pneumonia”. Images of the biopsy findings are shown in figures 1-4.
Q1. The histopathologic findings are:
- Sufficient to establish only a pattern diagnosis.
- Suspicious of an entity but require correlation with microbiology.
- Diagnostic.
- Diagnostic but in only the clinical and radiological context of the patient.
Q2. The dots observed in the frothy exudate correspond to:
- Cystic forms of a fungus.
- Anthracosis.
- Artifacts.
- Trophozoites.
Q3. Which of the following statements is TRUE:
- Pneumocystis pneumonia is typically encountered in HIV-positive patients.
- Pulmonary alveolar proteinosis (PAP) features a frothy exudate.
- In cryptococcal pneumonia, the dots of the exudate are diagnostic.
- Pulmonary edema is typical of the organizing phase of diffuse alveolar damage.
Answers to Quiz
Q2. D
Q3. A
Diagnosis
Discussion
These dots are the most important feature to distinguish PJP from other intraalveolar exudates such as edema, fibrin, or alveolar proteinosis. Intraalveolar macrophages can mix with the exudate, but other inflammatory cells are not usually prominent. The adjacent alveolar septa are variably thickened from chronic inflammation, hyperplasia of alveolar pneumocytes, and sometimes fibrosis. Unlike most other fungi, Pneumocystis has a cystic form (containing multiple sporozoites) and free trophozoites (which develop when sporozoites are released from mature cysts). Grocott Methenamine Silver (GMS) staining reveals cysts, 4- to 6-µm discs, “helmets” or “crushed ping-pong balls” but not free trophozoites. In cases that manifest as DAD or granulomas, in which the characteristic exudate is not observed, the morphology on GMS stains raises the differential diagnosis with Cryptococcus, but this fungus shows budding and is visible on H&E. It should be remembered that there may be more than one infection in immunosuppressed patients; the association of Pneumocystis with cytomegalovirus (CMV) infection is typical.
Take home message for trainees: A frothy exudate with dots is diagnostic of PJP. The diagnosis may not always be suspected on clinical grounds.
References
Contributors
Staff pathologist
Department of Pathology
HU Vall d’Hebron
Barcelona, Spain