Click here to see all images
March, 2021
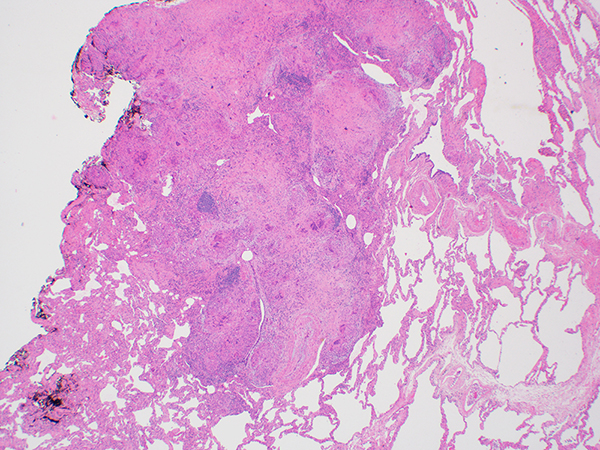
Case of the Month
Clinical History: A 64-year-old woman with worsening exertional dyspnea underwent a chest CT without contrast, which was described as showing moderate pulmonary fibrosis with probable centrilobular and paraseptal emphysema, and multiple, bilateral noncalcified lung nodules, measuring up to 1 cm. Her past medical history was most significant for severe developmental delay. She was a never smoker. A wedge biopsy of the lung was performed for evaluation of interstitial lung disease. H&E-stained sections are shown in Figures 1-5. AFB and GMS were negative (not shown). Immunostains for smooth muscle actin (SMA), estrogen receptor (ER) and HMB-45 are shown in Figure 6.
Quiz:
Q1. Which immunohistochemical stain, when positive, is the most helpful in evaluating the smooth muscle-like spindle cells and establishing the diagnosis?
- HMB-45
- Estrogen receptor
- Progesterpone receptor
- Smooth muscle actin
Q2. In the lung, the characteristic distribution of the granulomas in this entity is
- Random
- Lymphangitic
- Air-space centered
- Bronchiolocentric with cavitation
Q3. Which of the following would best explain the histologic findings?
- An atypical mycobacterial infection.
- Surreptitious smoking.
- A history of uterine leiomyoma
- Tuberous sclerosis complex
Answers to Quiz
Q2. B
Q3. D
Diagnosis
Discussion
In the current case, in addition to the granulomas, there are scattered cysts, some of which show subtle, focal collections of abnormal smooth-muscle like spindle cells within the cyst walls focally infiltrating the perivascular interstitium. Upon closer inspection, the spindle cells show centrally-located, oval nuclei and variably abundant, slightly vacuolated pale eosinophilic cytoplasm. This combination of features is diagnostic of lymphangioleiomyomatosis, a diagnosis supported by the presence of immunoreactivity for HMB-45. The differential diagnosis includes benign metastasizing leiomyoma. When cystic, BML tends to show a circumferential population of atypical spindle cells, in contrast to the localized aggregates in LAM. Additionally, benign metastasizing leiomyoma is positive for SMA and ER/PR, but negative for HMB-45.
Lymphangioleiomyomatosis is a rare disorder almost exclusively affecting women and frequently occurring in the setting of tuberous sclerosis complex. Other manifestations of tuberous sclerosis include neuropsychiatric symptoms and renal angiomyolipomas. Given the history of developmental delay in this patient, the possibility of tuberous sclerosis was raised, leading to subsequent discovery of a renal angiomyolipoma. Rare case reports describe coexistent sarcoidosis and lymphangioleiomyomatosis; however, the association is likely random.
Take home message: Immunohistochemistry for HMB-45 can be helpful in establishing a diagnosis of lymphangioleiomyomatosis, particularly when the diagnosis is unexpected.
References
Di Marco F, Palumbo G, Terraneo S, et al. Lymphangioleiomyomatosis, multifocal micronodular pneumocyte hyperplasia, and sarcoidosis: more pathological findings in the same chest CT, or a single pathological pathway? BMC Pulm Med 2017;17:107.
Johnson SR, Taveira-DaSilva AM, Moss J. Lymphangioleiomyomatosis. Clin Chest Med 2016;37:389-403.
Mukhopadhyay S, Gal AA. Granulomatous lung disease: an approach to the differential diagnosis. Arch Pathol Lab Med 2010;134:667-90.
Contributors
Assistant Professor of Thoracic Pathology
University of Michigan Ann Arbor, MI
Jeffrey L. Myers, MD
A. James French Professor of Diagnostic Pathology
University of Michigan Ann Arbor, MI