Click here to see all images
August, 2022
Case of the Month
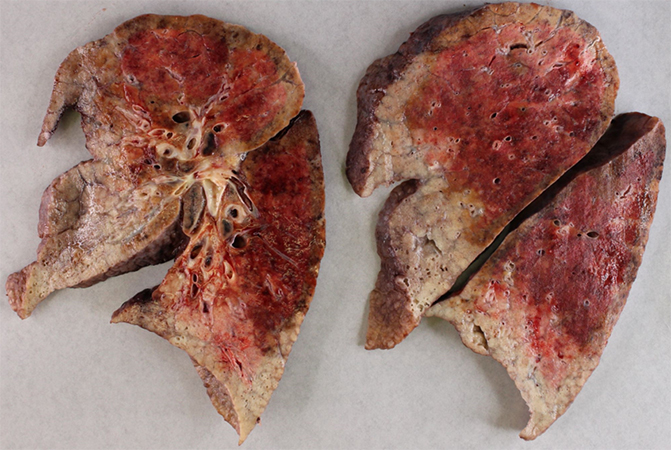
Clinical History: Fifty-plus year old adult woman admitted from outside institution for interstitial lung disease (ILD) with acute exacerbation (status post VATS wedge biopsy at outside institution with complicated hospital course and ICU admission for worsening acute lung injury/ARDS). Patient had been successfully cannulated and initiated on VV ECMO prior to transfer. Subsequently patient underwent bilateral orthotopic lung transplant (BOLT). No past medical history of any malignancy. No parenchymal or pleural masses or effusions reported on imaging studies. Gross image of native left lung (660 grams) is shown (Figure 1). No nodules, masses or pleural thickening seen on gross examination. Sections from left hilar lymph node are presented for evaluation (Figure 2) and few immunohistochemical stains performed to delineate clusters of cells with abundant eosinophilic cytoplasm seen in lymph node subcapsular sinus (Figure 3).
Q1. Differential diagnoses of these cells in lymph node subcapsular sinus include -
- Carcinoma cells
- Mesothelioma cells
- Melanoma cells
- Histiocytes or benign inclusions in lymph nodes
- All of the above
Q2. The clinical history, gross findings, histology and immunohistochemical staining results support these cells to be –
- Metastatic mesothelioma cells
- Metastatic carcinoma cells
- Mesothelial cell inclusions in lymph node
- None of the above
Q3. The hypotheses proposed to explain the presence of these cells in lymph nodes include
- Embryologic remnants
- Metaplastic changes
- Pleural inflammation/injury resulting in lymphatic dissemination/embolization
- All of the above
Answers to Quiz
Q2. C
Q3. C
Diagnosis
Discussion
Lymph node inclusions such as benign glandular inclusions, nevus cells, as well as decidua are known to occur in different regional lymph nodes. Mesothelial cell inclusions in mediastinal lymph nodes mimicking metastatic carcinoma was first reported by Brooks et al (1) in two patients with pleural effusions, secondary to presumed infectious etiology and to underlying lymphoma. Though rare, other authors have also reported this occurrence (2-4). Presence of pleural effusion secondary to underlying inflammatory or neoplastic etiologies has been a common finding in these studies. Hence, the hypothesis that pleural inflammation/injury giving rise to pleural effusions disrupt and dislodge these mesothelial cells into the subpleural lymphatic spaces, which are then carried over to mediastinal lymph nodes is favored. However, Rutty et al (2) found no keratin positive cells in 318 mediastinal lymph nodes removed for a variety of reasons, suggesting that this phenomenon has a low prevalence overall; and though benign mesothelial cells may reach the mediastinal lymph nodes, they may not survive for long in most circumstances.
Differential diagnoses considered includes metastatic carcinoma, metastatic mesothelioma, melanoma, as well as sinus histiocytosis and other benign inclusions in lymph nodes. Location of these mesothelial cells in subcapsular, trabecular or medullary sinuses without disrupting the lymph nodal parenchyma and no stromal response are essential morphologic features to favor benign mesothelial cell inclusions, along with clinical history, imaging findings, and immunohistochemical staining results, to rule out the other considerations in differential diagnosis.
References
Mesothelial cell inclusions within mediastinal lymph nodes. Rutty GN, Lauder I. Histopathology. 1994 Nov;25(5):483-7.
Embolization of mesothelial cells in lymphatics: the route to mesothelial inclusions in lymph nodes? Suárez Vilela D, Izquierdo García FM. Histopathology. 1998 Dec;33(6):570-5.
Benign mesothelial cells in mediastinal lymph nodes. Parkash V, Vidwans M, Carter D. Am J Surg Pathol. 1999 Oct;23(10):1264-9.
Contributors
Clinical Associate Professor
Department of Pathology and Laboratory Medicine
University of Pennsylvania
Founders 6.039
3400 Spruce Street
Philadelphia PA 19104