Click here to see all images
August, 2023
Case of the Month
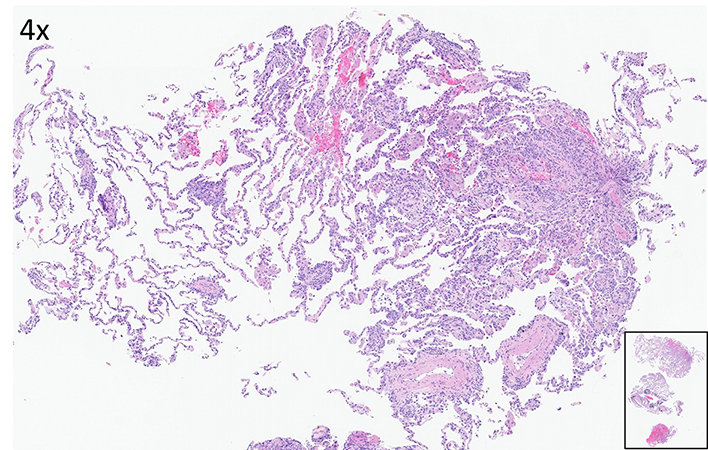
Clinical History: A 55-year-old man with a 40 pack-year smoking history who quit smoking recently. He presented with a short duration of malaise, weight loss and associated fever. The blood work-up was notable for blasts seen on the manual differential count. Flow cytometric analysis showed 80% myeloblasts supporting the diagnosis of acute myeloid leukemia. CT-chest imaging showed dense consolidation in the left upper lobe and lingual with scattered air bronchograms. Additional subpleural ground glass opacities anteriorly and laterally in the right middle lobe were also seen. Spiculated nodules in the upper and middle lobes were present. These changes were felt to be suspicious for acute pneumonia. Underlying atypical pneumonia or superimposed pulmonary edema cannot be excluded. Later, he underwent transbronchial cryobiopsy of the right upper lobe (Figures 1-5 H&E, IHC).
Q1. Which of the following is best diagnosis for this lesion?
- Neuroendocrine proliferations, including carcinoid tumor.
- Metastatic small blue round cell tumor.
- T-Lymphoblastic leukemia/lymphoma.
- Extramedullary acute myeloid leukemia.
Q2. Immunohistochemical profile of this lesion is best represented by:
- Cytokeratins (+), TTF-1 (+), synaptophysin (+)
- Cytokeratins (-),TTF-1 (-), desmin (+), Mart-1 (-)
- Cytokeratins (-),TdT (+), CD117 (+), CD4/CD8 (+)
- Cytokeratins (-), TdT (-), CD117 (+), CD43 (+)
Q3. According to the current WHO classification (5th edition) system, myeloid sarcoma is a mass forming proliferation of myeloblasts in an extramedullary site, while interstitial infiltration without a mass is called extramedullary acute myeloid leukemia.
- True
- False
Answers to Quiz
Q2. D
Q3. A
Diagnosis
Discussion
The most common involvement of the lung is by extranodal marginal zone lymphoma of mucosa associated lymphoid tissue (MALT lymphoma). Secondary involvement is much more common in the setting of advanced nodal or systemic hematolymphoid diseases which should always be considered in the differential diagnosis. In terms of the lung transplant setting, most posttransplant lymphoproliferative disorders included Epstein-Barr virus driven B-cell process, but extranodal marginal zone B-cell lymphoma of mucosa associated lymphoid tissue, monomorphic T/NK cell lymphomas, florid follicular hyperplasia and EBV negative lymphomas are also included in this category. Early histologic findings may consistently show atypical interstitial cells but typically present as a mass-like lesion in the lung. Additional comprehensive immunohistochemical work-up and hematopathology consultation would help in the definitive diagnosis. Our Patient also developed skin and CNS involvement simultaneously and receiving high-dose chemotherapy.
Take home message
Be aware of the extramedullary lung involvement by acute myeloid leukemia and transbronchial lung biopsy is useful to make the diagnosis.
References
2. Orazi A and Pileri SA In. WHO Classification of Thoracic Tumours, 5th Edition, Volume 5, 2021.
3. Aguilera N, Gru AA. Reexamining post-transplant lymphoproliferative disorders: Newly recognized and enigmatic types. Semin Diagn Pathol. 2018 Jul;35(4):236-246
Contributors
Assistant Professor of Pathology
Director, Pulmonary Pathology, and Immunohistochemistry
Virginia Commonwealth University Health
Richmond, VA