Click here to see all images
December, 2023
Case of the Month
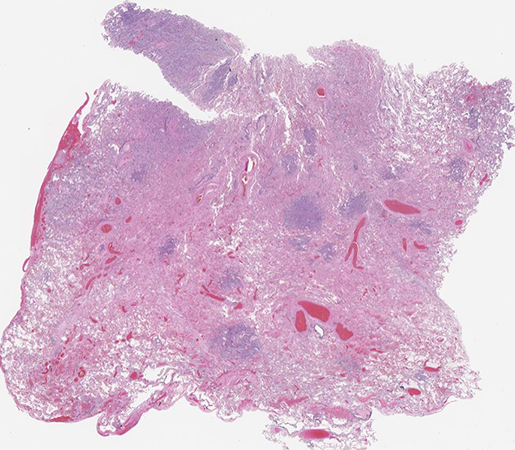
Clinical History: A 77-year-old man, heavy smoker, with history of chronic obstructive pulmonary disease with severe paraseptal emphysema, and recurrent pneumothoraces, who presented with cough and inspiratory chest pain, and was found to have a moderate left pneumothorax with a left upper lobe (LUL) consolidation. A LUL wedge resection was performed showing prominent multifocal micronodular epithelial cell proliferation (Figures 1-3). Immunohistochemical stains (IHC) showed the neoplastic cells to be positive for pancytokeratin (AE1/AE3), WT1, and calretinin (Figure 4), but negative for claudin-4, CEA, TTF-1, p40, CD163, S100, CD1a, ERG, CD31, SOX10, SMA and collagen IV. BAP1 expression was lost by IHC (Figure 5), and several asbestos bodies were identified on an iron stain (Figure 6).
Q1. Clinically and radiologically, what is the main differential diagnostic consideration?
- lymphangitic carcinomatosis
- interstitial lung disease
- miliary tuberculosis
- none of the above
Q2. Histologically, which of the following non-neoplastic lung diseases can this diagnosis mimic?
- desquamative interstitial pneumonia
- organizing pneumonia
- hypersensitivity pneumonitis
- all of the above
Q3. Which of the following findings would support this diagnosis?
- IHC expression of mesothelial markers in the absence of carcinoma markers
- BAP 1 loss by IHC and/or CDKN2A (p16) deletion by FISH
- electron microscopy showing long microvilli
- all of the above
Answers to Quiz
Q2. D
Q3. D
Diagnosis
Discussion
Patients with this tumor are most often middle aged to older men who present with non-specific symptoms, such as cough and shortness of breath. In a subset of reported cases, the patients have a known history of exposure to asbestos or radiation. This condition is often bilateral and predominantly shows multiple ground glass opacities and reticulation on imaging which can be mistaken for interstitial lung disease (Question 1). Occasionally this condition is associated with pleural effusion, blebs/bullae, or recurrent pneumothoraces.
Histology is characterized by multinodular proliferation of mildly atypical epithelioid cells with a variety of growth patterns mimicking adenocarcinoma, including lepidic, acinar, solid and micropapillary. Cytologically, the tumor cells are cuboidal and enlarged, and contain moderate eosinophilic or amphophilic cytoplasm with frequent prominent single central nucleoli. Lymphovascular invasion and lymph node metastases may be present. DIM can mimic a broad variety of conditions, with some cases having been described as morphologically similar to desquamative interstitial pneumonia, organizing pneumonia, pneumoconiosis, hypersensitivity pneumonitis, or Langerhans cell histiocytosis (Question 2).
Diagnostic workup of DIM is similar to pleural-based mesotheliomas and positivity for at least two mesothelial markers, such as WT1, calretinin, D2-40 and CK5/6, with negativity for at least two carcinoma markers, such as claudin-4, BerEp4, MOC31, CEA, and B72.3, is recommended to make the diagnosis (Question 3). As with its pleural counterpart, loss of BAP1 expression and/or homozygous loss of CDKN2A (p16) by FISH support the diagnosis, but are not required. Although not routinely performed, the mesothelial origin of these tumor cells can be further supported by the classic finding of long microvilli on electron microscopy.
The differential diagnosis includes multifocal primary or metastatic adenocarcinoma, multifocal micronodular pneumocyte hyperplasia (MMPH; in patients with tuberous sclerosis), and reactive pneumocyte changes in the context of interstitial lung disease. The key to identifying DIM is keeping this unusual condition in mind and recognizing the morphology of mesothelial cells so that confirmatory IHC can be performed.
The specific etiology of DIM is unknown. The clinical course reported in the limited series is aggressive, with similar outcomes and survival to the classic diffuse pleural mesothelioma.
Take home message for trainees:
In rare cases, mesothelioma can predominantly involve the lung parenchyma rather than the pleura. DIM most often presents with bilateral micronodular growth which can mimic interstitial lung disease on radiology. One should always keep the possibility of this diagnosis in mind when dealing with multifocal intrapulmonary epithelial proliferations.
References
Larsen BT, Klein JR, Hornychová H, et al. Diffuse intrapulmonary malignant mesothelioma masquerading as interstitial lung disease: a distinctive variant of mesothelioma. Am J Surg Pathol 2013;37:1555-64.
Larsen BT, Smith ML, Roden AC, et al. Molecular and Ultrastructural Features of Diffuse Intrapulmonary Malignant Mesothelioma. Am J Surg Pathol 2019;43:147-150.
Nind NR, Attanoos RL, Gibbs AR. Unusual intraparenchymal growth patterns of malignant pleural mesothelioma. Histopathology 2003;42:150-5.
RanYue W, ChunYan W, Likun H, et al. Diffuse intrapulmonary mesothelioma mimicking pulmonary lepidic adenocarcinoma: a rare case report and review of the literature. Diagn Pathol. 2023 May 16;18:64.
Contributors
Thoracic Pathology Fellow
Memorial Sloan Kettering Cancer Center, NY
Susan M Armstrong, MD, PhD
Thoracic Pathology Fellow
Memorial Sloan Kettering Cancer Center, NY
Marina K Baine, MD, PhD
Assistant Attending Pathologist
Memorial Sloan Kettering Cancer Center, NY