Click here to see all images
July, 2023
Case of the Month
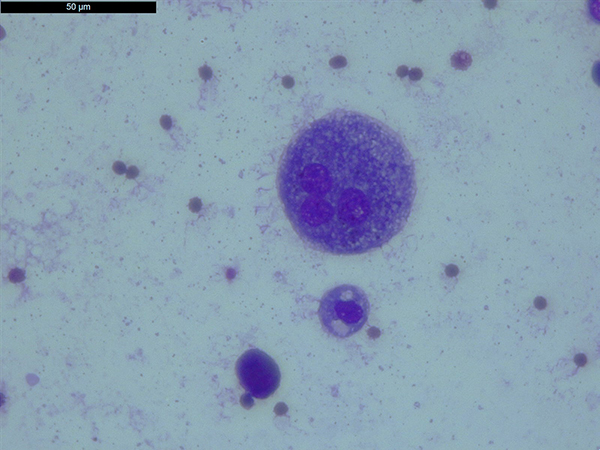
Clinical History: A 36-year-old man presented to our hospital with shortness of breath and a cough. From the clinical evaluation, the symptoms were more intense on the weekend (when he spent time in his country cottage), and although they persisted during the week, they were milder. The exact time of onset was not recalled by the patient but was probably 1 or 2 years ago. An HRCT was performed (Fig.1.), followed by a bronchoalveolar lavage (BAL) the BAL fluid was sent for cytology examination. Photomicrographs from the BAL fluid cytology May-Grünwald Giemsa (MGG) stain are shown in Figures 2-5.
Q1. : Which of these statements about hypersensitivity pneumonitis (HP) and BAL fluid lymphocytosis is false?
- Hypersensitivity pneumonitis is also known as extrinsic allergic alveolitis.
- Lymphocytosis in HP is often more than 50%, with moderate neutrophilia, modest eosinophilia, and mast cells.
- Levels of neutrophils in BAL increase with time after antigen exposure in HP.
- Foamy macrophages may be seen in the BAL fluid of patients with HP.
Q2.Which bird is not commonly associated with causing hypersensitivity pneumonitis, also known as Bird Breeder's Lung?
- Pigeons
- Owls
- Budgerigars (parakeets)
- Canary
Q3. What is the structure seen in figure 5?
- Ferruginous body
- Curschmann spiral
- Fungal hyphae
- feater barbule
Answers to Quiz
Q2. B - Only a few cases have been reported to be caused by native, uncaged birds such as owls.
Q3. D - This structure represents a feather barbule which is a lateral branch of a feather barb.
Diagnosis
Discussion
The HRCT of the patient revealed pleural thickening and fibrotic lesions with mixed subpleural patterns and traction bronchiectasis predominantly at the bilaterally level of the upper and basal lobes, without pathological pleuro-pericardial collections (Fig.1.). BAL fluid analysis was remarkable for a high percentage of 40% of lymphocytes (Fig.2.), high numbers of lipid-laden alveolar macrophages (Fig.3.), and a few multinucleated giant cells (Fig.4.). Additionally, upon revision of the slides, feather barbules were identified with hooklets approximately 100 μm apart (Fig.5.). Following a multidisciplinary discussion, a diagnosis of hypersensitivity pneumonitis was rendered. The patient was interviewed for possible exposure to feathers and admitted that he made his own pillows from the geese he grew at his country cottage. In hypersensitivity pneumonitis (HP) the upper lungs may exhibit diffuse centrilobular nodules of ground-glass attenuation, which can be seen bilaterally. In the lower lungs, there can be a combination of ground-glass opacities, a mosaic pattern, and normal lung tissue. This combination is often referred to as the "head-cheese sign". In our case the HRCT pattern was atypical and the use of BAL fluid cytology was diagnostic. BAL fluid cytology in HP can often be impressive for the high count of lymphocytes especially if the BAL is performed after acute exposure to the antigenic stimulus. A high percentage of lymphocytosis in BAL fluid, more than 50% is diagnostic for HP if coupled with typical clinical and image presentation on HRCT. Here, the patient’s BAL lymphocytosis of 40%, with signs of mucostasis (presence of a high number of lipid-laden alveolar macrophages), and the presence of feather barbules, and the clinical interview of exposure was sufficient for a diagnosis of HP.
Take home message for trainees: BAL fluid cytology is important, especially in cases where HRCT patterns are atypical. Always view the entire slide and always integrate your microscopic findings with the clinical information.
References
Davidson K, Ha D, Schwarz M, et al. bronchoalveolar lavage as a diagnostic procedure: a review of known cellular and molecular findings in various lung diseases. Journal of Thoracic Disease 2020;Sep;12:4991.
Patolia S, Tamae Kakazu M, Chami HA, et al. bronchoalveolar lavage lymphocytes in the diagnosis of hypersensitivity pneumonitis among patients with interstitial lung disease. Annals of the American Thoracic Society 2020;Nov;17:1455-67.
Contributors
Thoracic pathologist
Spitalul Clinic de Boli Infecțioase și Pneumoftiziologie Dr. Victor Babeș
Timișoara, Romania.