Click here to see all images
June, 2023
Case of the Month
Clinical History: A 57 year old man presented with shortness of breath, cough and swelling of face and neck since 6 months. Chest CT revealed an anterior mediastinal mass of size 1.8 cm in greatest dimension accompanied by enlarged mediastinal lymph nodes. A CT guided core needle biopsy was performed and sent for histopathological examination. Photomicrographs from the biopsy are shown in Figures 1-7 (Figures 1-3: H&E, Figure 4: INSM1, Fig 5: PAX8, Fig 6: TTF1, Fig 7: Ki67).
Q1. Following are the essential diagnostic criteria for atypical thymic carcinoid tumors except:
- Neuroendocrine morphology
- Mitotic count 2-10 mitoses/2mm2
- Absence of any necrosis
- All of the above
Q2.Which of the following histopathologic features would not be considered common for atypical Thymic carcinoid ?
- Solid and diffuse growth pattern
- Nuclear molding, crush artefacts
- Tumor necrosis
- Lymphovascular invasion
Q3. Thymic carcinoids are associated with which of the following syndromes?
- Lynch syndrome
- Li-Fraumeni syndrome
- Birt-Hogg-Dubé syndrome
- MEN 1 syndrome
Answers to Quiz
Q2. B
Q3. D
Diagnosis
Discussion
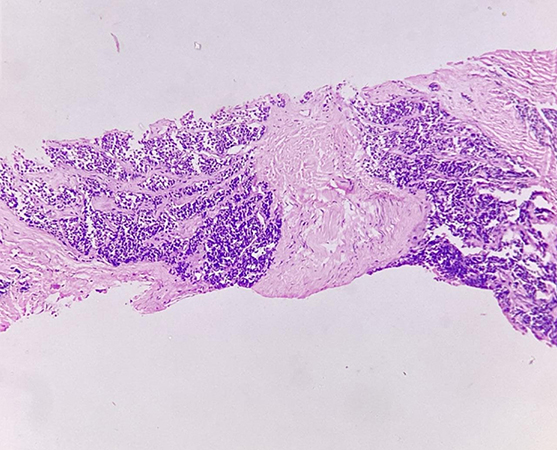
The biopsy shows linear cores of tissue demonstrating a tumor arranged predominantly in the form of solid nests with surrounding stroma (Fig 1). These nests are separated by delicate vasculature (Fig 2) . Focal areas of palisading are noted. Individual tumor cells are uniformly small, round to oval to spindle shaped with scant cytoplasm and finely dispersed chromatin and inconspicuous nucleoli. Few scattered atypical large cells are present . No areas of necrosis are noted in the tissue submitted. Miotic activity is 4 per 2 mm2 (Fig 3). INSM1 (Fig 4) and PAX 8 (Fig 5) show nuclear positivity TTF1 is negative (Fig 6) and Ki67 is around 15% (Fig 7). The final diagnosis was atypical carcinoid tumor of thymic origin.
Thymic neuroendocrine tumous are a rare form of thymic neoplasms, accounting for only 2-5% of cases. The World Health Organization (WHO) has classified neuroendocrine neoplasms of the thymus into three categories based on their grade: low, intermediate, and high. The low-grade category consists of typical carcinoids, which have no necrosis and less than two mitoses per 2 mm2. The intermediate-grade category corresponds to atypical carcinoids, which have necrosis present (any) and/or 2-10 mitoses per 2 mm2. The high-grade category has more than 10 mitoses per 2mm2 and is further divided into two subcategories: large cell neuroendocrine carcinoma (NEC), which has non-small cell cytology and NEC markers, and small cell NEC, which has small cell cytology and more than 10 mitoses per 2mm2. Most thymic neuroendocrine tumors belong to the intermediate atypical carcinoid subgroup. Around 25% of the thymic carcinoid tumors have a family history of multiple endocrine neoplasia type 1 (MEN1).
Patients with carcinoid tumors typically present with local symptoms such as chest pain, cough, dyspnea, or superior vena cava syndrome. Approximately one-third of patients also experience paraneoplastic manifestations, including Cushing syndrome, hypercalcemia/hypophosphatemia, the Syndrome of Inappropriate ADH Secretion, and other rarer symptoms like carcinoid syndrome. Around 50% of patients develop regional lymph node or distant metastasis, with bone and lungs being the most common sites.
Histopathology shows a typical neuroendocrine architectural and cytological pattern. The tumors contain small, uniform, round to oval cells with salt and pepper chromatin arranged in festoons, trabeculae, rosettes, and glandular structures. A delicate neuroendocrine tumor-type vasculature between the nests and trabeculae is characteristic. Atypical carcinoids often show some degree of nuclear pleomorphism, focal diffuse growth pattern, and desmoplastic stroma. Even a small punctate area of necrosis in an otherwise typical carcinoid is sufficient for a diagnosis of atypical carcinoid.
Carcinoid tumors are immunoreactive for keratins (AE1/AE3, CAM 5.2), neuroendocrine markers like INSM1, Synaptophysin, Chromogranin, and CD56. Most carcinoids express at least two of these neuroendocrine markers in more than 50% of tumor cells. Ki-67 helps in grading the tumors. A subset of thymic carcinomas can be positive for Pax8, however, this is most commonly seen with polyclonal Pax8 antibodies and is less common with monoclonal antibodies.
The main differential diagnosis for thymic neuroendocrine tumors includes metastatic pulmonary neuroendocrine tumors, which can be differentiated using TTF1 and PAX8 (TTF1 is positive in pulmonary neuroendocrine tumors, and PAX8 is positive in subset of thymic neuroendocrine tumors). However, in many cases this can be challenging and clinical history and imaging findings can be helpful. Thymomas with spindle cell morphology (Type A thymomas) can be differentiated with neuroendocrine markers. Paragangliomas can be distinguished with cytokeratin and S100. Medullary thyroid carcinoma can be differentiated based on positivity for calcitonin and carcinoembryonic antigen.
Tumor stage (TNM system) has been found to be an important prognostic factor. Most studies show that atypical carcinoids of the thymus are aggressive and Radical resection of the primary tumor with local lymph nodes followed by post operative Radiotherapy is the standard of care.
Take home message for trainees: Thymic neuroendocrine tumors are rare neoplasms They should be classified into low, intermediate and high grade tumors using the WHO classification criteria ; they also need to be differentiated from metastatic neuroendocrine tumors (especially pulmonary neuroendocrine carcinomas) and other anterior mediastinal tumors using clinical, radiological, morphological and immunohistochemical features
References
Annikka W, Ximing T, Ignacio I W et all. Comparative immunohistochemical analysis of pulmonary and thymic neuroendocrine carcinomas using PAX8 and TTF-1. Mod Pathol. (2013) 26, 1554–1560
Cesar A.M, Saul S. Neuroendocrine Carcinomas (Carcinoid Tumor) of the Thymus: A Clinicopathologic Analysis of 80 Cases. Am J Clin Pathol. 2000 Jul;114(1):100-10.
Shan Z, Zhong-Tang W, Wen-Zhi L et al. Invasive atypical thymic carcinoid: three case reports and literature review. Onco Targets Ther. 2016; 9: 6171–6176.
Contributors
Founder Director, Consultant Pulmonary Pathologist
Association of Thoracic Pathologists
Mumbai, Maharashtra, India