Click here to see all images
July, 2019
Case of the Month
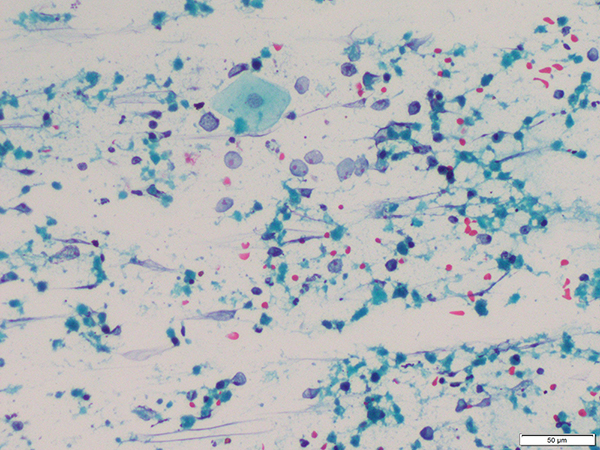
Clinical History: A 58-year old man presented with dry cough. He was a non-smoker with a history of diabetes on treatment. Contrast enhanced computed tomography showed consolidation of the left lower lobe of lung with bronchial narrowing, mediastinal lymphadenopathy and left-sided pleural effusion. Endobronchial ultrasound-guided transbronchial needle aspiration (Figures 1 and 2) and an endobronchial biopsy (Figures 3 and 4) were performed. Immunostains shown are p40 (Figure 5) and NUT (Figure 6).
Quiz:
Q1. Which of the following is true about this tumor?
- It exclusively arises in midline locations
- Abrupt squamous differentiation is characteristic
- Cytoplasmic positivity for anti-NUT antibody is confirmatory
- The clinical course is indolent with good outcome
Q2. Which of the following immunostains are usually positive in this tumor? (a) p40, (b) p63, (c) synaptophysin, (d) SALL4, (e) TTF-1, (f) pan-cytokeratin and (g) NUT
- (a), (b), (f), (g)
- (c), (e), (f)
- (a), (b), (d), (f)
- (f), (g)
Q3. Regarding cytomorphology, which of the following is FALSE?
- Tumor cells with dense cytoplasm suggestive of squamous differentiation is a very common finding
- Tumor cells are singly dispersed with scant cytoplasm, round to oval nuclei, and single small conspicuous nucleolus
- Nuclear molding can be seen
- Karyorrhectic debris and mixed inflammatory cells are frequently seen in the background
Q4. True or False: Cytomorphological features of this tumor are relatively non-specific and confirmatory diagnosis requires additional immunohistochemical or molecular testing
Answers to Quiz
Q2. A
Q3. A
Q4. True
Diagnosis
Discussion
NUT (nuclear antigen in testis) carcinoma, originally termed NUT midline carcinoma, is a highly aggressive type of squamous cell carcinoma that predominantly originates in the midline structures of the upper aerodigestive tract and mediastinum. With increasing reports of its occurrence in non-midline locations such as abdomen, lacrimal gland and iliac bone, the nomenclature has been changed to NUT carcinoma. Primary pulmonary NUT carcinoma accounts for less than 1% of lung cancer with less than 20 cases reported to date. These cases present at an advanced stage with frequent bony metastases and are associated with extremely poor outcome.
NUT carcinomas are defined by rearrangements involving the NUTM1 gene located at 15q14 that result in fusion with a member of the bromodomain-containing protein (BRD) family, usually BRD4 located on chromosome 19. These tumors are morphologically and immunohistochemically undifferentiated and are composed of primitive tumor cells with high mitotic indices. Focal and abrupt squamous differentiation adjacent to undifferentiated tumor cells is characteristic but is usually focal. Due to their undifferentiated morphology, these tumors have a high likelihood of being misdiagnosed. NUT carcinomas are diffusely positive for p63 or p40 (Fig 4) and cytokeratin, but nearly always negative for neuroendocrine markers and TTF-1. Immunohistochemistry using monoclonal NUT antibody is highly specific and sensitive for the diagnosis of NUT carcinoma (at a cut-off of >50% tumor cell staining) and shows a speckled staining pattern in tumor cell nuclei. Germ cell tumors may show focal NUT expression; however, NUT carcinomas are always negative for other germ cell markers such as SALL4 and OCT4.
In aspirates, the tumor cells are usually singly dispersed as naked nuclei or with a thin rim of cytoplasm, frequently associated with karyorrhectic debris and neutrophilic infiltration. 3-dimensional clusters with nuclear molding can also be seen. Nuclear chromatin is fine to coarse granular and usually shows a single conspicuous nucleolus. Presence of cells with dense cytoplasm representing tumor cells showing squamous differentiation, and frankly dyskeratotic cells are rare findings. Tumor cells with cytoplasmic vacuolation and multinucleation have also been described. The cytomorphological features of NUT carcinoma show considerable overlap with other small round cell tumors, and immunohistochemistry for NUT or molecular testing is invariably required for confirmation of diagnosis.
Take home message for trainees: NUT carcinomas are rare but highly aggressive malignancies that are frequently misdiagnosed due to overlapping morphological features. A high index of suspicion is necessary for accurate diagnosis, the latter being essential for prognostication and treatment decisions.
References
Kakkar A, Antony VM, Irugu DVK, et al. NUT midline carcinoma: A series of five cases, including one with unusual clinical course. Head Neck Pathol 2018;12(2):230-6.
Sholl LM, Nishino M, Pokharel S, et al. Primary pulmonary NUT midline carcinoma: clinical, radiographic, and pathologic characterizations. J Thorac Oncol 2015;10:951-9.
Contributor
Senior Research Associate
Department of Pathology
All India Institute of Medical Sciences
New Delhi, India
Deepali Jain, MD, FIAC
Associate Professor
Department of Pathology
All India Institute of Medical Sciences
New Delhi, India